Percutaneous Coronary Intervention (PCI) is a groundbreaking medical procedure that saves countless lives each year. Also known as coronary angioplasty, this minimally invasive technique opens blocked arteries in the heart, restoring crucial blood flow during critical cardiac events.
The procedure is essential in treating two life-threatening conditions:
During PCI, interventional cardiologists insert a thin catheter through blood vessels, usually starting from the wrist or groin. At the site of the blockage, they inflate a small balloon to widen the artery and often place a stent to keep it open.
Research shows the life-saving impact of PCI:
Time is critical in cardiac emergencies - every minute without proper blood flow can cause permanent heart damage. PCI's ability to quickly restore circulation makes it an essential tool in modern cardiac care, offering hope to patients facing life-threatening heart conditions.
In such emergencies, understanding and implementing the 6 adult chain of survival can greatly improve patient outcomes. This includes immediate actions like Basic Life Support (BLS) and Advanced Cardiac Life Support (ACLS), which are vital skills for anyone involved in emergency care.
Moreover, for healthcare providers looking to enhance their skills in these areas, there are comprehensive ACLS & BLS recertification courses available that include extensive resources and guaranteed pass options.
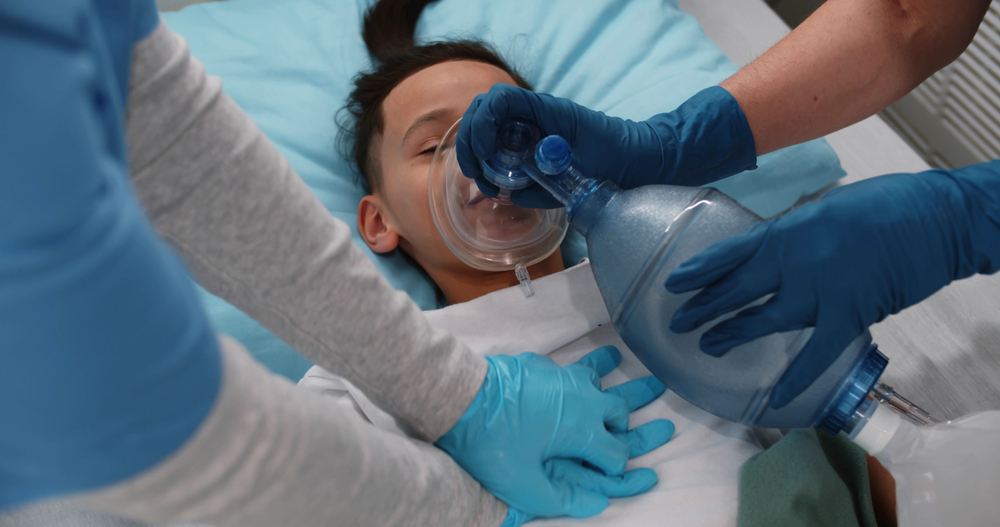
Additionally, it's important to note that pediatric patients may require different approaches during such emergencies. The Pediatric Basic Life Support Algorithm provides crucial guidelines for handling such situations effectively when two or more rescuers are present.
Acute Coronary Syndrome represents a spectrum of life-threatening heart conditions caused by reduced blood flow to the heart muscle. ACS manifests in three distinct forms:
The relationship between ACS and cardiac arrest is direct and potentially fatal. When coronary arteries become blocked, the heart muscle starves of oxygen, triggering:
These changes can rapidly progress to life-threatening arrhythmias and sudden cardiac arrest. Research shows that approximately 25-30% of ACS cases lead to cardiac arrest, with STEMI patients facing the highest risk.
The time between symptom onset and medical intervention is critical. Each minute without treatment increases the risk of:
Recognition of early warning signs becomes crucial for survival. Common symptoms include:
These symptoms demand immediate medical attention, as rapid diagnosis and treatment significantly improve survival rates and reduce complications.
In such scenarios, having basic life support (BLS) knowledge can be invaluable. For instance, understanding how to perform CPR can significantly increase the chances of survival during a cardiac arrest situation. If you're interested in enhancing your skills in this area, consider enrolling in an online BLS course through Affordable ACLS.
Moreover, it's essential to recognize that these health emergencies can occur not only in adults but also in children. Therefore, being equipped with Pediatric Advanced Life Support (PALS) skills can be extremely beneficial. This includes knowing how to respond during common household hazards, which often lead to accidents requiring immediate medical attention.
Understanding the implications of Acute Coronary Syndrome and its potential progression to cardiac arrest is vital. Early recognition of symptoms and immediate medical intervention can save lives. Furthermore, acquiring BLS and PALS certifications can equip individuals with the necessary skills to handle such emergencies effectively.
PCI works through a precise, minimally invasive approach to restore blood flow in blocked coronary arteries. The procedure begins with the insertion of a thin, flexible catheter into a blood vessel, typically through the wrist or groin area. Using X-ray guidance, your healthcare provider threads this catheter through your blood vessels until it reaches the blocked coronary artery.
The PCI Process:
The balloon angioplasty component of PCI physically pushes the plaque against the artery walls, creating immediate blood flow improvement. Modern stents, particularly drug-eluting versions, release medications that prevent the artery from re-narrowing, maintaining long-term vessel patency.
Key Benefits of PCI:
The restoration of blood flow through PCI triggers a cascade of positive effects. Your heart muscle receives the oxygen it desperately needs, preventing further tissue death. This rapid reperfusion helps preserve heart function and reduces the formation of scarring that could lead to future complications.
Studies show PCI success rates reaching 95% in experienced centers. The procedure's effectiveness lies in its ability to provide immediate mechanical relief of the blockage while simultaneously setting up conditions for long-term artery health through stent placement.
Modern PCI techniques incorporate advanced imaging technologies and specialized devices that enhance precision and safety. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) allow doctors to visualize the blocked artery from the inside, ensuring optimal stent placement and expansion.
However, it's important to note that while PCI is a critical intervention during Acute Coronary Syndrome (ACS) episodes, it's not a standalone solution. Following PCI, patients may require additional treatment strategies such as ACLS algorithms for comprehensive cardiac care. These algorithms provide structured guidelines for managing various cardiovascular emergencies effectively.
Moreover, recertification courses are essential for healthcare professionals to stay updated with the latest protocols and practices in advanced cardiac life support. Such continuous education ensures that medical personnel are well-equipped to handle emergencies related to heart conditions.
In addition to these educational resources, quizzes serve as effective tools for reinforcing knowledge and assessing competency in ACLS protocols. They can be especially useful after completing lessons such as the lesson on stroke management, which is crucial given that strokes can often accompany severe cardiac events.
The impact of successful PCI extends beyond the immediate procedure. Patients often experience significant improvement in their quality of life, with reduced ang
Time is muscle when it comes to treating myocardial infarction (MI). Research shows that for every 30-minute delay in performing PCI, the one-year mortality risk increases by 7.5%.
Key Time Metrics for PCI Success:
These metrics highlight the importance of immediate medical intervention. Recognizing the symptoms of a heart attack, such as chest tightness, nausea, or shortness of breath, is crucial. In such cases, it's essential to call 911 immediately and be prepared to start CPR if necessary. More information on heart attack symptoms and initial response can be found here.
PCI success rates in treating acute myocardial infarction are remarkable, with clinical studies reporting:
The effectiveness of PCI varies based on the type of myocardial infarction:
ST-Elevation MI (STEMI)
Non-ST Elevation MI (NSTEMI)
The introduction of drug-eluting stents has revolutionized MI treatment outcomes:
Real-world data from major cardiac centers demonstrates that patients receiving prompt PCI experience:
These impressive statistics underscore why PCI has become the gold standard treatment for myocardial infarction, particularly in facilities equipped with 24/7 cardiac catheterization laboratories.
To ensure that medical professionals are well-equipped to handle such emergencies, it's vital they undergo rigorous training. For instance, [BLS certification](https://affordableacls.com/lessons/2-solo-provider-adult-bls) provides essential skills for managing cardiac arrests until professional help arrives. Furthermore, understanding the latest guideline changes in emergency care can significantly improve patient outcomes.
The role of timely intervention and proper training cannot be overstated in the management of myocardial infarctions. It's also worth noting that [early coronary angiography and revascularization](https://www.ahajournals.org/doi
PCI plays a transformative role in patient outcomes after achieving Return of Spontaneous Circulation (ROSC). Research shows that patients who undergo PCI following out-of-hospital cardiac arrest have significantly lower in-hospital death rates compared to those who don't receive the treatment.
The timing of PCI after ROSC directly affects survival rates and neurological outcomes:
Post-cardiac arrest care protocols now routinely include PCI as a standard treatment, recognizing its crucial role in patient recovery. These protocols usually involve:
The presence of a comatose state after ROSC does not prevent coronary angiography or PCI. Studies show that unconscious patients who receive timely PCI experience:
Modern cardiac care facilities have specialized "Code ROSC" protocols in place, ensuring smooth coordination between emergency departments and catheterization laboratories. These protocols have reduced the time it takes to perform balloon angioplasty by an average of 30 minutes, resulting in:
The combination of therapeutic hypothermia with PCI has shown promising results in preserving neurological function. This approach protects both the heart and brain during the critical period after cardiac arrest.
For comprehensive guidance on managing post-cardiac arrest situations, including mastering the Post Cardiac Arrest Algorithm, it's essential to equip oneself with life-saving skills and expert knowledge.
Moreover, while moving victims is generally not recommended unless there is an immediate danger to their life, certain situations may require it. Understanding the best practices for moving victims can be crucial in such scenarios.
In recent years, the impact of AI on emergency cardiac care has been transformative, improving diagnosis, treatment precision, and patient outcomes through advanced data analysis and real-time decision support.
For those working with children, obtaining a PALS certification could provide valuable skills necessary for handling emergencies like sudden cardiac arrest. Familiarity with PALS primary and secondary surveys is crucial for such situations.
Lastly, having access to clear and concise [ACLS algorithms](https://affordableacls.com/acls-algorithms

PCI procedures carry inherent risks that medical professionals must carefully manage. Understanding these complications helps healthcare providers implement preventive measures and deliver optimal patient care.
Modern technological advancements have revolutionized PCI procedures, significantly reducing complication rates and improving patient outcomes. Drug-eluting stents (DES) represent a groundbreaking innovation in coronary artery disease treatment. These specialized devices release anti-proliferative medications directly into the arterial wall, preventing tissue overgrowth and reducing restenosis rates to less than 5%.
The introduction of radial artery access has transformed PCI procedures. This approach reduces bleeding complications by 73% compared to femoral access, allowing faster patient recovery and earlier discharge. Specialized closure devices for femoral access cases have also enhanced safety profiles.
Pre-procedure risk assessment protocols, which include assessing the patient's overall health and specific cardiovascular risks, are crucial in minimizing potential complications.
Advanced hemodynamic support devices now provide temporary cardiac assistance during high-risk PCIs. These tools maintain vital organ perfusion while allowing interventionalists to complete complex procedures safely.
The integration of artificial intelligence in PCI planning helps identify optimal intervention strategies, predict potential complications, and guide stent selection. Machine learning algorithms analyze patient-specific factors to customize treatment approaches and improve procedural success rates.
Percutaneous Coronary Intervention (PCI) is a crucial part of modern heart care. It has completely changed how we treat Acute Coronary Syndrome and patients who have just had their hearts restarted after cardiac arrest. This procedure can open up blocked arteries and restore blood flow, turning what used to be life-threatening situations into manageable medical emergencies.
The benefits of PCI go beyond just saving lives:
Studies consistently show that hospitals with the ability to perform PCI right away have better outcomes for their patients. When advanced techniques are used alongside skilled healthcare professionals, PCI becomes an essential lifeline during heart emergencies.
In cases where adult tachycardia with a pulse occurs, acting quickly with PCI can make a significant difference. This condition often requires immediate action to restore normal heart function, something that PCI can achieve effectively.
The methods used in PCI are constantly evolving, pushing the limits of what's possible in heart care. From stents that release medication to improved procedures, each new development makes this critical treatment option even stronger. For individuals facing life-threatening heart issues, PCI is more than just a medical procedure – it's an opportunity for a new lease on life, made possible by the precision of modern medicine.
.jpg)

