Post-cardiac arrest syndrome consist of five phases, which includes the immediate phase (20 minutes after the return of spontaneous circulation [ROSC]), early phase (from 20 minutes to 6–12 hours after ROSC), intermediate phase (from 6–12 to 72 hours after ROSC), recovery phase (3 days after ROSC), and rehabilitation.
For the purposes of ACLS, the Adult Post Cardiac Arrest algorithm covers primarily the immediate phase.
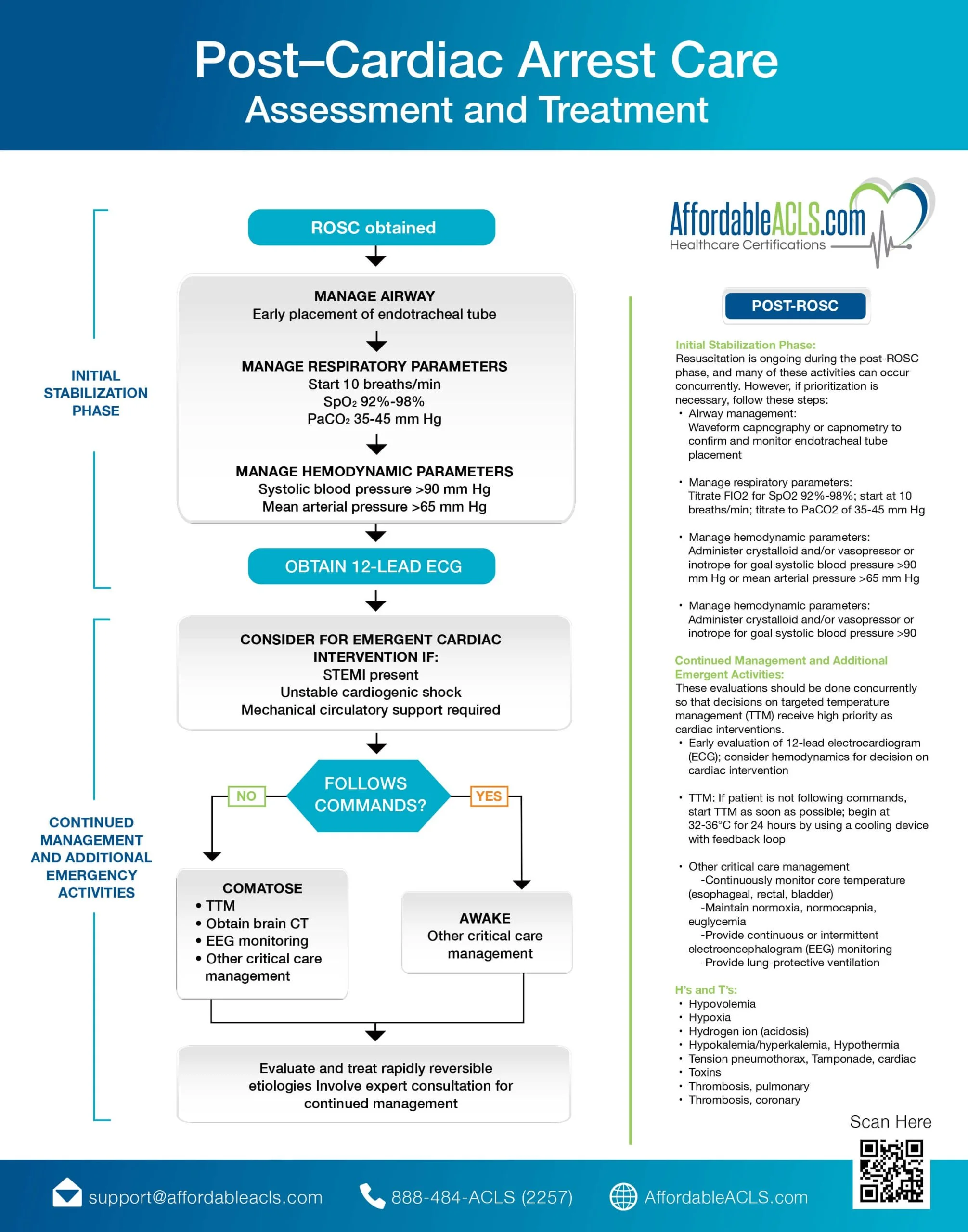
A. Achieve a return of spontaneous circulation (ROSC). Return of spontaneous circulation (ROSC) is the return of a detectable pulse and blood pressure. As the first step, this is a critical component of the resuscitation process because it indicates to you that the heart has resumed function and the vital organs are once again receiving oxygen. Immediate management of post-cardiac care after the return of spontaneous circulation can improve survival rates and functional recovery in the patient. You can achieve ROSC through several approaches, though the most common are CPR or defibrillation (both techniques you will learn more about in your ACLS online course).ROSC is critical, but there is much more involved in post-cardiac arrest treatment, That’s because patients who reach ROSC are at higher risk for complications such as brain injury, organ dysfunction, and sepsis. They require close monitoring and ongoing care, as outlined in the post-cardiac arrest algorithm, to improve their future outcome
B. Optimize ventilation and oxygenation. According to post-cardiac arrest guidelines, you should start with 10 breaths a minute, and use the lowest inspired oxygen concentration necessary to maintain SATs of 94% or greater. Use continuous waveform capnography to confirm and monitor the correct placement of the ET tube if needed. Avoid hyperventilation or the condition in which a person breathes faster or deeper than is necessary for the body’s oxygen demand. Hyperventilation can cause a severe drop in carbon dioxide (CO2) levels in the blood, a condition called respiratory alkalosis.
C. Treat Hypotension (SBP <90 mm Hg). Check the patient’s blood pressure and treat for hypotension if needed. This is a condition where systolic blood pressure is less than 90. To do so, first, obtain IV access if it’s not already established, and verify the patency of the IV lines. Then treat the hypotension with IV bolus and vasopressor infusion. At this stage, consider treating any reversible causes that may have precipitated the cardiac arrest. These could include:
D. Obtain a 12 lead ECG: STEMI. Obtain a 12 lead ECG as soon as possible after the return of spontaneous circulation to identify patients with STEMI or a high suspicion of acute myocardial infarction (AMI).
E. Begin coronary reperfusion. If STEMI is detected, EMS personnel should transport the patient to an appropriate facility quickly to reduce the time to treatment. Hospital personnel should begin coronary reperfusion with percutaneous coronary intervention (PCI).
F. Check for an ability to follow commands. If STEMI or AMI are not detected, determine the patient’s ability to follow commands. Depending on if they are still comatose or awake, choose the following procedures.
If comatose: Initiate targeted temperature management (TTM). If the patient is unable to follow commands or respond in a meaningful way, the high-performance team should initiate TTM.
If awake: Transfer to advanced critical care. Once TTM has been initiated, or if the patient is responsive and able to follow commands, the patient should be transferred to advanced critical care as soon as possible to undergo further medical review and management.
Go at your own pace. Schedule the exam at your convenience. Manage your certification process from the convenience of your home or workspace. Achieving certification has never been this convenient.