Myocardial ischemia is a serious heart condition where the heart muscle doesn't get enough blood and oxygen. This lack of blood flow can lead to severe problems, such as heart attacks and dangerous irregular heartbeats.
The main tool used to diagnose myocardial ischemia is the electrocardiogram (ECG). This simple yet powerful test measures the heart's electrical activity and shows specific patterns that indicate reduced blood flow to the heart. These patterns help doctors:
In this detailed guide, you'll learn everything you need to know about interpreting ECGs for myocardial ischemia. You'll discover:
Knowing these ECG patterns can be critical in emergency situations. Whether you're a medical student, healthcare worker, or someone interested in heart health, this guide will give you the skills to spot and understand ECG changes in myocardial ischemia.
But recognizing these changes is only one aspect of managing myocardial ischemia. Responding quickly to a heart event is crucial, and understanding the adult chain of survival is vital for anyone involved in emergency care.
Additionally, medical professionals should be familiar with Basic Life Support (BLS) and Advanced Cardiac Life Support (ACLS) procedures. These abilities are essential when handling heart emergencies caused by myocardial ischemia. For those needing recertification, our ACLS & BLS recertification bundle for groups provides an all-inclusive solution.
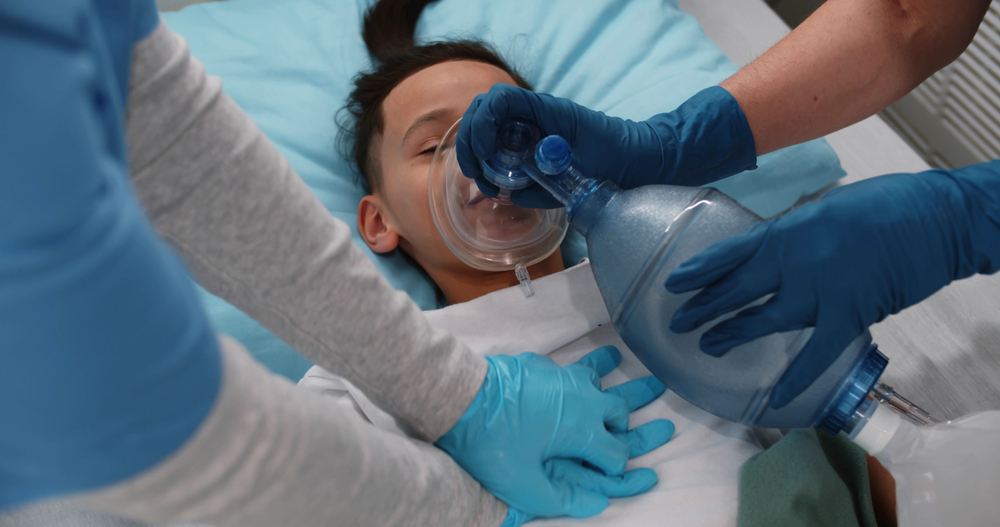
In cases involving children, the approach varies slightly. Understanding the Pediatric Basic Life Support Algorithm, particularly when two rescuers are available, can greatly enhance outcomes in such situations. This algorithm addresses crucial aspects like ensuring scene safety, performing compressions and ventilation, using an AED, and activating the EMS system.
While it's essential to grasp the ECG patterns associated with myocardial ischemia, acquiring life-saving abilities through BLS and ACLS training is just as crucial.
Your heart muscle requires a constant supply of oxygen-rich blood to function properly. When this blood flow becomes restricted or blocked, you're experiencing myocardial ischemia - a condition that can lead to serious cardiac complications.
At its core, myocardial ischemia develops when your heart's oxygen demand exceeds its supply. This imbalance typically occurs due to:
These two distinct types of cardiac ischemia affect different layers of your heart muscle:
Myocardial ischemia presents with several key symptoms:
Left untreated, myocardial ischemia can progress to:
Understanding these patterns helps medical professionals identify the severity and extent of cardiac damage, guiding critical treatment decisions in acute settings.
In such emergencies, having basic life support (BLS) skills can be invaluable. Consider enhancing your knowledge with resources like affordableacls.com, which offers comprehensive study materials for BLS certification.
Moreover, it's essential to recognize that while we often think about adult health emergencies, children are also at risk for certain situations at home. Familiarizing yourself with common household hazards and emergency responses can make a significant difference in ensuring their safety.
An electrocardiogram (ECG or EKG) records your heart's electrical activity through electrodes placed on your skin. This vital diagnostic tool captures the heart's electrical impulses, translating them into waveforms that medical professionals can interpret.
A standard ECG uses 12 different leads to view your heart's electrical activity from multiple angles:
Each lead provides a unique perspective of your heart's electrical activity, helping identify specific areas of concern or damage.
A healthy ECG displays specific measurements:
A normal ECG shows:
The art of ECG interpretation requires understanding these basic elements and their relationships. Medical professionals analyze these components systematically, looking for patterns that might indicate various cardiac conditions, including myocardial ischemia.
In emergency situations where immediate medical attention is required, understanding how to effectively interpret an ECG can be crucial. For instance, when moving victims during such emergencies, it's generally not recommended unless there's a direct danger to their life or if necessary for providing care. In such cases, assisting an unconscious victim who is breathing and has a pulse into the recovery position can protect their airway and reduce the risk for aspiration. Learn more about moving victims during emergencies.
Additionally, healthcare providers must stay updated with the latest practices and procedures in emergency care. This often involves participating in recertification courses which cover essential topics including advanced cardiac life support (ACLS) algorithms that are vital in managing cardiac emergencies.

Understanding specific ECG components helps identify myocardial ischemia early and accurately. Each wave pattern tells a unique story about the heart's electrical activity during ischemic events.
These ECG components create distinct patterns during myocardial ischemia. The ST segment shifts reflect ongoing injury currents, while T wave changes signal early ischemic events. Q waves develop as permanent markers of damaged heart tissue. Recognizing these specific alterations enables rapid diagnosis and appropriate intervention strategies.
In such critical situations where myocardial ischemia is suspected, it's essential to be equipped with the right ACLS algorithms that simplify emergency care training and improve life-saving skills effectively. Additionally, having a solid understanding of BLS certification can be invaluable during these emergencies.
For those preparing for such certifications, employing the best study tips for online course takers can significantly enhance learning outcomes. It's also important to stay updated with any guideline changes related to ACLS and BLS protocols.
Moreover, understanding the relationship between myocardial ischemia and stroke is crucial as both conditions can have overlapping risk factors and symptoms. For an in-depth understanding of this connection, refer to the lesson on stroke.
To gain a comprehensive understanding of how to interpret these critical ECG components such as the P wave, QRS complex, ST segment, and T wave in relation to myocardial ischemia, you may find this detailed guide on how to read an ECG particularly useful. Furthermore, familiarizing
When myocardial ischemia occurs, specific patterns on an electrocardiogram (ECG) indicate the severity and extent of damage to the heart muscle. These changes follow a predictable sequence, reflecting the progressive nature of cardiac injury.
Transmural ischemia affects the entire thickness of the heart muscle wall, resulting in distinct ECG changes that require immediate medical attention. The underlying process unfolds in several stages:
The changes observed on the ECG are caused by electrical currents flowing between damaged and healthy areas of the heart muscle (myocardium). During transmural ischemia:
Key Diagnostic Features:
ST Elevation Criteria:
Early Recognition Signs:
These ECG changes indicate severe injury to the heart muscle requiring immediate restoration of blood flow (reperfusion therapy). The presence of hyperacute T waves serves as an early warning sign, often preceding the need for advanced management strategies such as those covered in our PALS Certification. Early recognition and intervention are crucial to minimize further damage and improve patient outcomes.
Subendocardial ischemia affects the inner third of the heart muscle wall, resulting in specific ECG patterns that are different from transmural ischemia. This type of injury happens when a decrease in blood flow only impacts the endocardial layer of the myocardium.
The typical ECG findings associated with subendocardial ischemia include:
The underlying mechanism leads to specific electrical alterations:
You will most often observe these patterns in:
The absence of ST elevation sets NSTEMI/unstable angina apart from STEMI, but these ECG changes still indicate significant damage to the heart muscle. The depth of ST depression is directly related to how severe the ischemia is - deeper depressions point to more extensive involvement of the subendocardium.
It's important to identify certain key patterns:
Precise diagnostic criteria help clinicians identify myocardial ischemia on ECG with confidence. These standardized measurements serve as reliable indicators for diagnosis and treatment decisions.
These quantitative criteria form part of a comprehensive ECG analysis. The presence of multiple criteria strengthens diagnostic confidence and helps determine the extent of myocardial involvement.
A systematic approach to 12-lead ECG interpretation helps identify myocardial ischemia accurately. Here's a step-by-step method to analyze ECGs when you suspect cardiac ischemia:
This structured analysis helps you avoid missing subtle signs of ischemia and ensures consistent interpretation across different clinical scenarios. Remember to integrate these findings with the patient's clinical presentation and cardiac biomarkers for accurate diagnosis.
In cases of suspected myocardial ischemia, it's crucial to recognize the symptoms of a heart attack which may include chest tightness, nausea, sweating, shortness of breath, fatigue, pain in the arm or jaw, and pallor. Immediate action is essential: call 911, have the patient chew one full-strength aspirin, and be prepared to start CPR if necessary. The heart attack is usually caused by a clot that occludes a coronary artery leading to ischemia.
Acute coronary syndromes present distinct ECG patterns that serve as crucial diagnostic markers. Understanding these patterns enables rapid identification and appropriate treatment selection.
These patterns reflect different degrees of myocardial injury. STEMI indicates complete coronary occlusion requiring immediate intervention, while NSTEMI/unstable angina patterns suggest partial or intermittent blockage needing urgent evaluation.
ECG findings directly influence critical treatment decisions in myocardial ischemia. The speed and accuracy of ECG interpretation can mean the difference between life-altering outcomes for patients experiencing acute coronary events.
The ECG serves as a dynamic tool throughout treatment, guiding medication adjustments and identifying complications. Continuous ECG monitoring helps detect reperfusion arrhythmias and recurrent ischemia, allowing for rapid intervention when needed.
Mastering ECG interpretation in myocardial ischemia is a critical skill for every healthcare professional involved in cardiac care. The ability to recognize subtle ECG changes can make the difference between life and death for patients experiencing acute coronary events.
Your systematic approach to ECG analysis should include:
The confidence to interpret ECGs comes through dedicated practice and continuous learning. Each ECG tells a unique story of the heart's electrical activity, and your expertise in reading these patterns transforms into immediate, life-saving interventions for patients.
In situations such as post-cardiac arrest, having a solid grasp on the Post Cardiac Arrest Algorithm can be invaluable. Similarly, understanding the Adult Tachycardia with a Pulse Algorithm will equip you with essential skills for managing critical situations effectively.
Key takeaways for clinical practice:
Remember: Your skill in ECG interpretation directly impacts patient outcomes. The time invested in perfecting this fundamental diagnostic tool pays dividends in improved patient care and clinical decision-making. Make ECG interpretation a cornerstone of your clinical expertise, and embrace each ECG as an opportunity to refine your diagnostic abilities.
It's also worth noting that advancements in technology, particularly AI, are significantly enhancing our approach to emergency cardiac care. For instance, AI is transforming emergency cardiac care by improving diagnosis, treatment precision, and patient outcomes through advanced data analysis and real-time decision support.
Lastly, if you're regularly working with children, obtaining a PALS certification could be beneficial. It equips you with the necessary skills to handle not just cardiac arrest situations but also other medical emergencies such as allergic reactions or medication side-effects. Understanding the PALS Primary And Secondary Surveys is crucial in these scenarios.
.jpg)

