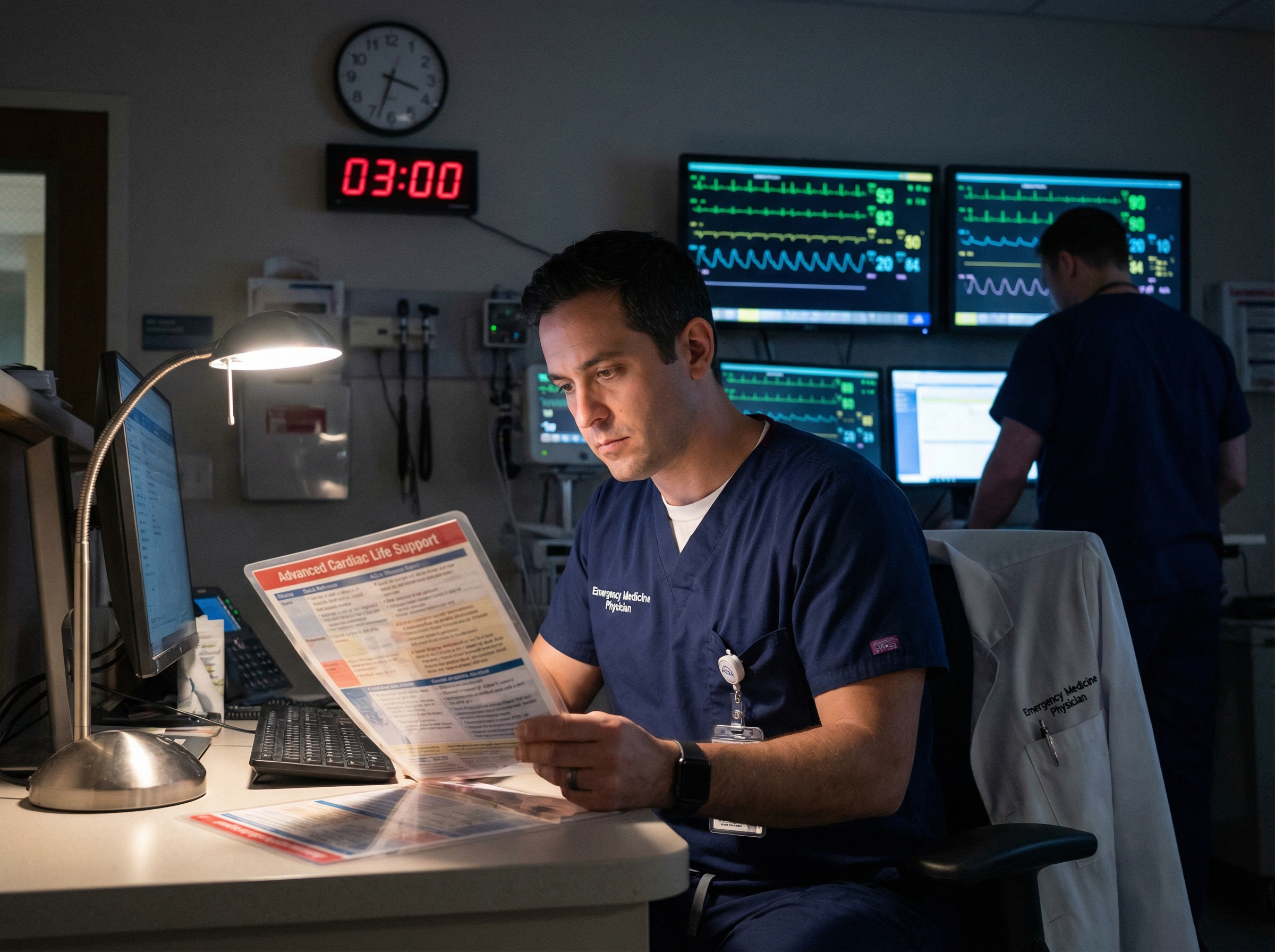
It's 3:47 AM. You're six hours into your night shift in the emergency department when the overhead speakers crackle to life: "Code Blue, ED Bay 4." Your body feels heavy, your mind momentarily foggy from circadian disruption, but your patient needs you now. This is the reality for thousands of healthcare professionals who staff our hospitals during the overnight hours, and it's precisely why having a streamlined ACLS toolkit designed for night shift conditions isn't just helpful—it's essential.
Research from studies on emergency medicine night shift performance reveals a sobering truth: working a series of night shifts results in substantial cognitive decline, with emergency physicians scoring an average of 11.9 points lower on cognitive assessments during night shifts compared to day shifts. When you're managing a cardiac arrest at 4 AM, you can't afford to rely solely on mental acuity that may be compromised by sleep deprivation and circadian misalignment. You need quick reference strategies, muscle memory protocols, and fatigue-resistant systems that work when you're running on empty.
Before we dive into specific ACLS strategies, it's crucial to understand what's actually happening to your body and brain during night shifts. This knowledge helps you work with your physiology rather than against it.
Your circadian rhythm is your body's internal 24-hour clock, regulating everything from body temperature and hormone release to alertness and reaction time. When you work nights, you're forcing yourself to be awake when your circadian drive for alertness is at its lowest and trying to sleep when it's at its highest. According to the CDC's research on shift work and circadian rhythms, this opposition to natural biological rhythms leads to shortened and disrupted sleep, excessive sleepiness while awake, and critically—increased errors in the workplace and greater risk of accidents.
The peak danger zone occurs during the second half of your night shift, typically between 3 AM and 6 AM, when your body temperature drops to its lowest point and melatonin levels remain elevated. This is exactly when your cognitive performance, reaction time, and decision-making capacity are most compromised—and unfortunately, when many cardiac emergencies occur.
The research on night shift performance in emergency medicine is extensive and concerning. Studies show that emergency physicians sleep significantly less after night shifts compared to day shifts—an average of 5 hours and 13 minutes versus 6 hours and 20 minutes. This sleep deficit translates directly into measurable performance decrements: vigilance reaction times slow, procedural skills like intubation take longer, and short-term memory declines by approximately 15 percent.
Perhaps most relevant to ACLS providers, research on emergency medicine residents found that proximity to night shifts negatively impacted performance on simulated resuscitations, particularly in the critical domain of communication. When you're managing a code, clear communication with your team isn't optional—it's the difference between a coordinated resuscitation and chaos.
Given the cognitive challenges of night shift work, your toolkit needs to compensate for fatigue-related performance decrements. The goal is to reduce cognitive load and create automatic, reflexive responses to common ACLS scenarios.
When a cardiac arrest occurs at 2 AM and you're fighting circadian-induced brain fog, you don't want to waste precious seconds trying to recall algorithm details from memory. Your adult cardiac arrest algorithm should be immediately accessible—whether that's a laminated card in your scrub pocket, a quick-access bookmark on your phone, or posted prominently in your code cart area.
The same applies to your bradycardia management algorithm and tachycardia algorithm. Night shift is not the time to rely on perfect recall. Create redundancy in your reference systems: digital backup, physical backup, and visual cues in your environment.
Medication errors increase with fatigue, and the stakes are incredibly high during ACLS scenarios. A comprehensive ACLS medications cheat sheet should be part of your standard night shift setup. This reference should include not just dosages, but also routes of administration, indications, contraindications, and the timing of repeat doses.
Key medications to have immediately referenced include epinephrine (1 mg IV/IO every 3-5 minutes), amiodarone (300 mg first dose for refractory VF/pVT, 150 mg second dose), atropine for symptomatic bradycardia, and adenosine for stable SVT. When you're fatigued, even familiar medications can momentarily slip your mind. External references eliminate this risk.
Modern ACLS providers have an advantage previous generations didn't: powerful clinical decision support tools in their pockets. Quality ACLS apps for smartphone quick reviews can provide algorithm walkthroughs, medication calculators, and even timers to help you maintain proper CPR cycles and medication intervals.
The key is familiarizing yourself with these tools during your well-rested day shifts, so they become second nature when you need them at 4 AM. Practice navigating to critical information quickly. Some apps offer offline functionality—essential if you work in areas with poor cellular reception or where hospital WiFi is unreliable.
Your ACLS toolkit isn't complete without strategies to maintain cognitive performance throughout your shift. These evidence-based interventions can help you stay sharper when it matters most.
Strategic napping isn't a sign of weakness—it's a performance enhancement tool backed by substantial research. According to studies on healthcare worker fatigue management, reductions in fatigue scores by 20 to 35 percent have been documented through strategic napping. Even brief naps of 10 to 20 minutes during breaks can counteract fatigue, though the ideal duration for night shift naps is up to 45 minutes to avoid sleep inertia.
If your facility provides call rooms or break areas conducive to rest, use them strategically. The optimal nap timing is typically during your natural circadian dip between 2 AM and 4 AM. Set an alarm to prevent oversleeping, and consider drinking caffeine immediately before your nap—by the time it takes effect 15 to 20 minutes later, you'll be waking up with a double boost of alertness.
What you eat during your night shift directly impacts your cognitive performance and energy stability. Heavy, high-glycemic meals cause blood sugar spikes and crashes that exacerbate fatigue. Instead, focus on balanced meals and snacks with complex carbohydrates and protein—oatmeal with nuts, whole grain toast with eggs, Greek yogurt with berries, or vegetables with hummus.
Research suggests that favoring low-glycemic index foods during night shifts helps prevent metabolic disturbances without negatively affecting glycemic profiles. Pack healthy snacks before your shift: fresh fruit, nuts, string cheese, and cut vegetables. Avoid the temptation of vending machine candy bars or excessive caffeine—both create dependency cycles that worsen overall alertness.
Hydration is equally critical. Dehydration impairs cognitive function and can mimic or worsen fatigue symptoms. Keep a water bottle with you and set reminders to drink regularly throughout your shift. Aim for at least 8 ounces per hour, adjusting for activity level and environment.
Light is the most potent regulator of your circadian rhythm, which means you can use it strategically to enhance night shift alertness. Bright, blue-enriched light during your shift helps signal to your brain that it should be awake and alert. Many emergency departments are already brightly lit, but if you work in areas with dimmer lighting, consider using a portable bright light therapy device during breaks.
Equally important is managing light exposure after your shift. Wear sunglasses during your morning commute home to minimize sunlight exposure and reduce melatonin suppression. This helps preserve your ability to fall asleep once you're home. Blackout curtains, eye masks, and creating a dark sleep environment during the day are essential for quality recovery sleep.
ACLS scenarios are inherently team-based, and fatigue affects everyone on your night shift crew. Understanding how to optimize team performance under these conditions is crucial.
Closed-loop communication becomes even more critical during night shifts. This technique—where the receiver repeats back the message to confirm understanding—creates a built-in error-checking system that compensates for fatigue-related miscommunication. During a code, this sounds like: "John, give 1 mg of epinephrine IV." John responds: "Giving 1 mg epinephrine IV now," and then confirms after administration: "1 mg epinephrine given IV."
This redundancy might seem excessive during calm, well-rested conditions, but at 3 AM when cognitive function is compromised, it catches errors before they reach the patient. Make closed-loop communication a non-negotiable standard for your night shift codes.

Ambiguity is the enemy of fatigued teams. When a code is called, immediate and explicit role assignments eliminate confusion and cognitive load. The team leader should quickly designate: compressor, airway manager, medication administrator, recorder, and runner. Use names, not assumptions: "Sarah, you're on compressions. Mike, you manage the airway. Jennifer, you're giving medications."
This clarity allows each team member to focus their limited cognitive resources on their specific responsibilities rather than wondering what they should be doing or whether someone else is handling a critical task.
High-quality CPR is exhausting under any circumstances, but during night shifts when baseline fatigue is already elevated, compressor fatigue sets in even faster. Strict adherence to two-minute compressor rotations isn't optional—it's essential for maintaining the compression depth and rate that gives your patient the best chance of survival.
Designate someone to watch the clock or set a timer. The incoming compressor should be positioned and ready to swap seamlessly when the two minutes are up. This prevents the dangerous decline in compression quality that occurs when fatigued providers try to push through "just a little longer."
Running ACLS codes on night shift isn't just physically demanding—it takes a psychological toll that accumulates over time. Building sustainable practices protects your long-term career and well-being.
After managing a difficult code during your night shift, your instinct might be to just move on to the next patient or task. Resist this urge. A brief debriefing—even just five minutes—helps process the emotional impact, identifies learning opportunities, and provides team support. This is especially important during night shifts when you may have fewer colleagues available for informal processing.
Effective debriefings don't need to be lengthy or formal. Gather your team, acknowledge what was difficult, highlight what went well, identify one or two areas for improvement, and check in on how everyone is feeling. This practice builds resilience and team cohesion while preventing the accumulation of unprocessed trauma.
Night shift workers often feel isolated from the broader healthcare community, which typically operates on day schedules. Intentionally building peer support networks among your fellow night shift providers creates understanding, validation, and practical support from colleagues who truly understand the unique challenges you face.
This might look like a regular group chat, monthly meetups for coffee, or simply checking in on each other after difficult shifts. According to mental health strategies for ACLS providers, establishing peer support groups and access to mental health resources is crucial for long-term wellness in high-stress healthcare roles.
Research shows that 58 percent of emergency medicine physicians report that night shift work negatively influences job satisfaction, with 43 percent indicating that night shifts have caused them to consider leaving emergency medicine entirely. Common effects include chronic fatigue, poor quality sleep, mood changes and irritability, and health maintenance challenges.
Be honest with yourself about how night shifts are affecting your health, relationships, and job satisfaction. If you're experiencing persistent sleep problems, significant mood changes, health deterioration, or thoughts of leaving your profession primarily due to night shifts, it may be time to discuss schedule modifications with your employer or consider transitioning to a different shift pattern. Your long-term health and career sustainability matter more than pushing through indefinitely.
Beyond managing actual codes during your night shifts, you need to maintain current ACLS certification—a challenge when most traditional certification courses operate on day schedules that conflict with your sleep needs.
If you work primarily night shifts, attending an 8 AM ACLS recertification class after working all night—or giving up precious sleep time on a day off—isn't just inconvenient; it's a setup for poor learning retention and potential safety issues driving to and from class while sleep-deprived.
This is precisely why time-flexible online certification matters for night shift nurses and other healthcare providers. Online ACLS certification allows you to complete required training when your body and brain are actually capable of learning—not when you're fighting circadian misalignment and sleep deprivation.
With platforms like Affordable ACLS, you can complete your certification or recertification entirely online, at your own pace, breaking the material into manageable chunks that fit your unique schedule. Study during your natural peak alertness hours, take breaks as needed, and complete the certification when it works for your body's rhythm—not an arbitrary class schedule.
When preparing for ACLS certification or recertification as a night shift worker, strategic timing of your study sessions matters tremendously. Avoid trying to study immediately after a night shift when your cognitive function is at its lowest. Instead, study after you've had adequate recovery sleep, ideally during your circadian peak alertness hours.
For most people, even those adapted to night shift, peak cognitive function occurs during late morning to early afternoon hours. Schedule your study sessions during these windows when possible. Break the material into smaller chunks rather than attempting marathon study sessions—your fatigue-management-adapted brain will retain information better with distributed practice.
Take advantage of unlimited retake policies offered by quality online certification providers. If you don't pass an exam on your first attempt because you misjudged your alertness level or scheduled study during a suboptimal time, you can retake without financial penalty once you're better prepared.
Knowledge without implementation is just theory. Here's how to operationalize everything we've discussed into a practical pre-shift routine that sets you up for success.
Before each night shift, run through this systematic checklist to ensure you're prepared for any ACLS scenario that might arise:
Your optimal night shift ACLS toolkit will evolve based on your experience, work environment, and personal physiology. After each shift—especially after managing ACLS scenarios—take a few minutes to reflect on what worked well and what could be improved.
Did you struggle to remember a medication dose that should have been on your cheat sheet? Add it. Did a particular app prove unhelpful in the heat of the moment? Replace it. Was there a communication breakdown with your team? Debrief and establish a new protocol. This continuous improvement approach builds a personalized system that gets stronger with each shift.
Working night shifts as an ACLS provider is undeniably challenging. The circadian disruption, cognitive fatigue, and physical toll are real and well-documented. But with the right toolkit—combining quick reference resources, fatigue mitigation strategies, optimized team dynamics, and attention to mental health—you can provide excellent care even when you're running on empty.
Remember that preparation is your greatest ally against fatigue. When your brain isn't functioning at full capacity, external systems compensate. Your laminated algorithms, medication cheat sheets, smartphone apps, and practiced team communication protocols become cognitive prosthetics that ensure quality care regardless of what time the code is called.
Most importantly, recognize that choosing sustainable practices isn't just about being a better clinician tonight—it's about being able to continue providing excellent care for years to come. Protect your sleep, nourish your body, support your mental health, and build systems that work with your physiology rather than against it. Your patients, your team, and your future self will thank you.
And when your certification renewal comes due, choose options that respect your unique schedule and circadian needs. You're already working hard enough during your shifts—your professional development shouldn't require sacrificing the recovery sleep that makes safe, effective night shift work possible.
.jpg)

