When a child experiences cardiac arrest, every second counts. The BLS Pediatric Cardiac Arrest Algorithm for multiple rescuers represents a critical framework that can mean the difference between life and death.
This comprehensive guide explores the essential components of pediatric cardiac arrest management through a multi-rescuer approach. You'll learn:
This article equips you with the knowledge to implement this life-saving protocol effectively, whether you're a healthcare professional or a certified rescuer working in team-based emergency scenarios.
Pediatric cardiac arrest occurs when a child's heart stops pumping blood effectively throughout the body. This life-threatening condition requires immediate medical intervention to prevent death or severe neurological damage.
The anatomical and physiological differences in children create specific challenges:
Recognizing these distinct characteristics helps healthcare providers and rescuers deliver appropriate, age-specific care during cardiac arrest events. The successful management of pediatric cardiac arrest requires specialized knowledge, proper training, and quick action.
For instance, mastering the Post Cardiac Arrest Algorithm can significantly improve outcomes in such critical situations. Additionally, obtaining proper certification through recertification courses can equip healthcare professionals with essential life-saving skills.
To ensure a thorough understanding of pediatric resuscitation, engaging in quizzes such as this lesson review or this general quiz can be highly beneficial.
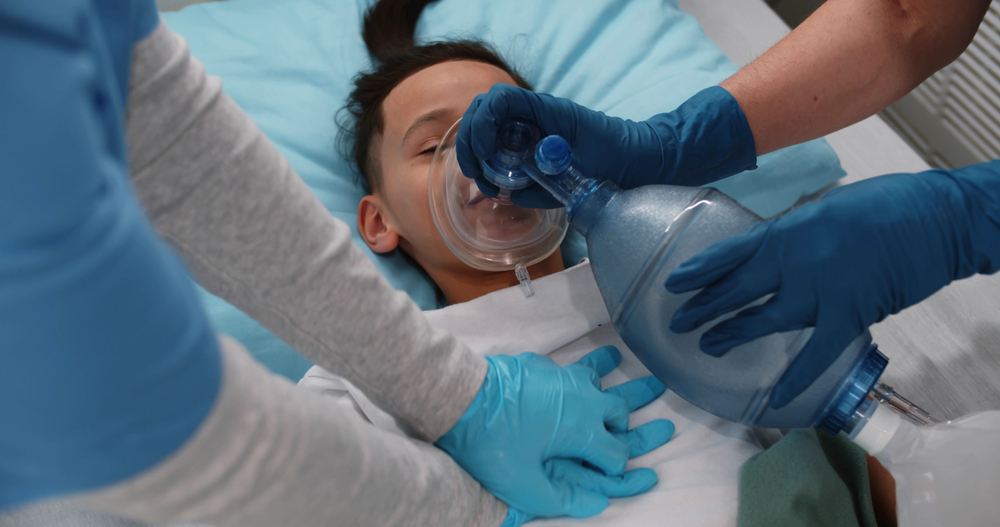
Cardiopulmonary Resuscitation (CPR) is a life-saving technique used during cardiac arrest to keep blood flowing to vital organs. It involves combining chest compressions with artificial ventilation to sustain life until professional medical help arrives.
High-quality CPR requires proper hand placement, adequate compression depth, appropriate rate, and minimal interruptions. Regular practice helps maintain these essential skills for emergency situations.
In certain scenarios, such as a heart attack, recognizing symptoms early can be crucial. Symptoms may include chest tightness, nausea, sweating, shortness of breath, fatigue, pain in the arm or jaw, and pallor. In such cases, it's important to call 911, have the patient chew one full-strength aspirin if possible, and be prepared to start CPR if necessary.
Basic Life Support in pediatrics follows specific protocols designed for children's unique anatomical and physiological needs. The BLS algorithm adapts core life-saving techniques to accommodate different age groups:
The pediatric BLS algorithm emphasizes rapid recognition of cardiac arrest and immediate initiation of high-quality chest compressions. This systematic approach maximizes survival chances through organized, efficient care delivery.
It's essential to stay updated with the latest guideline changes in BLS protocols to ensure effective response during emergencies. For those looking to refresh their skills, our BLS Recertification resources provide a comprehensive overview and practice questions to reinforce learning.
For detailed insights into the Pediatric Basic Life Support protocols, it's recommended to review the latest updates from authoritative sources such as the AHA 2020 pediatric BLS guidelines.

Multiple rescuers working together create a dynamic system that significantly improves the chances of survival during pediatric cardiac arrest. The coordinated efforts allow for continuous, high-quality CPR while managing additional critical tasks.
The multi-rescuer approach transforms individual efforts into a synchronized response system. Each team member's specific role assignment creates a clear chain of command, eliminating confusion and reducing time delays in critical interventions. This structured teamwork allows for rapid assessment, efficient resource utilization, and optimal delivery of life-saving care to pediatric patients.
The BLS Pediatric Cardiac Arrest Algorithm follows a precise sequence of actions designed for optimal patient outcomes. Here's the detailed protocol for multi-rescuer teams:
For those looking to refresh their skills in these crucial areas, consider an ACLS & BLS Recertification Bundle which includes comprehensive training and resources.
The seamless transition from Basic Life Support (BLS) to Advanced Life Support (ALS) marks a critical phase in pediatric resuscitation. BLS providers create the foundation for successful ALS interventions through:
The BLS team's role evolves during ALS integration - from primary care providers to essential support members. This partnership creates a comprehensive resuscitation effort, combining basic life-saving measures with advanced medical interventions.
For more detailed guidance on ACLS algorithms, which can simplify emergency care training and improve life-saving skills effectively, visit Affordable ACLS. Additionally, understanding solo provider adult BLS can further enhance the effectiveness of the initial response in both pediatric and adult cases.
Proper certification in Pediatric BLS and PALS algorithms is essential for providing effective resuscitation care to children. Healthcare professionals must keep their certifications active through recognized institutions to stay updated with the latest evidence-based practices.
Key Components of Pediatric Resuscitation Training:
The ever-changing nature of pediatric emergency care requires continuous improvement of skills. Research indicates that BLS and PALS skills can decline within 3-6 months after initial training, making regular recertification necessary.
Enrolling in an online PALS course through a recognized provider can greatly enhance your skills, ensuring you are fully prepared to handle various situations that may arise when working with children.
Certification Requirements:
Healthcare facilities often require PALS certification for staff working in:
Regular participation in mock codes and team-based scenarios helps maintain readiness and builds confidence in real emergency situations. These structured learning environments allow practitioners to improve their skills without endangering patient safety.
It's important to remember that PALS certification is not just about managing cardiac arrests. It also provides professionals with the necessary skills to handle other emergencies such as allergic reactions or medication side effects, which are common in pediatric patients. Additionally, understanding post-resuscitation management is vital for ensuring the child's ongoing well-being after initial treatment.

Multi-rescuer pediatric resuscitation presents unique challenges that can impact the effectiveness of emergency response. Here are critical obstacles and practical solutions:
In addition, conducting regular simulation training helps teams identify and overcome these challenges while building effective coordination patterns for real emergencies.
The BLS Pediatric Cardiac Arrest Algorithm for multiple rescuers is an important framework that improves pediatric resuscitation outcomes. Research shows that coordinated team efforts significantly increase survival rates in pediatric cardiac arrest cases.
The success of this approach depends on:
The multi-rescuer approach creates a strong system where individual strengths combine to form an effective emergency response unit. Healthcare providers who master these protocols contribute to a larger mission: saving young lives during critical cardiac events.
Your commitment to understanding and implementing these protocols makes a difference. Each successful resuscitation reinforces the power of teamwork in pediatric emergency care. The BLS Pediatric Cardiac Arrest Algorithm serves as your guide to delivering optimal care when every second counts.
.jpg)

