Atrial fibrillation (AFib) is the most common heart rhythm disorder, affecting millions of people worldwide. It disrupts the heart's normal electrical signals, leading to irregular and often rapid heartbeats that can greatly affect one's quality of life.
Key Statistics:
Effectively managing AFib is crucial to prevent severe complications like stroke and heart failure. Proper treatment can alleviate symptoms, enhance heart function, and reduce hospitalization rates.
The main goals of AFib management are:
These objectives are usually achieved through a combination of medications known as atrial drugs. Each class of medication targets specific aspects of AFib management, working together to create a comprehensive treatment approach.
Understanding your AFib medication options empowers you to participate actively in your treatment journey. This guide explores the various classes of atrial drugs, their uses, benefits, and considerations to help you make informed decisions about your heart health.
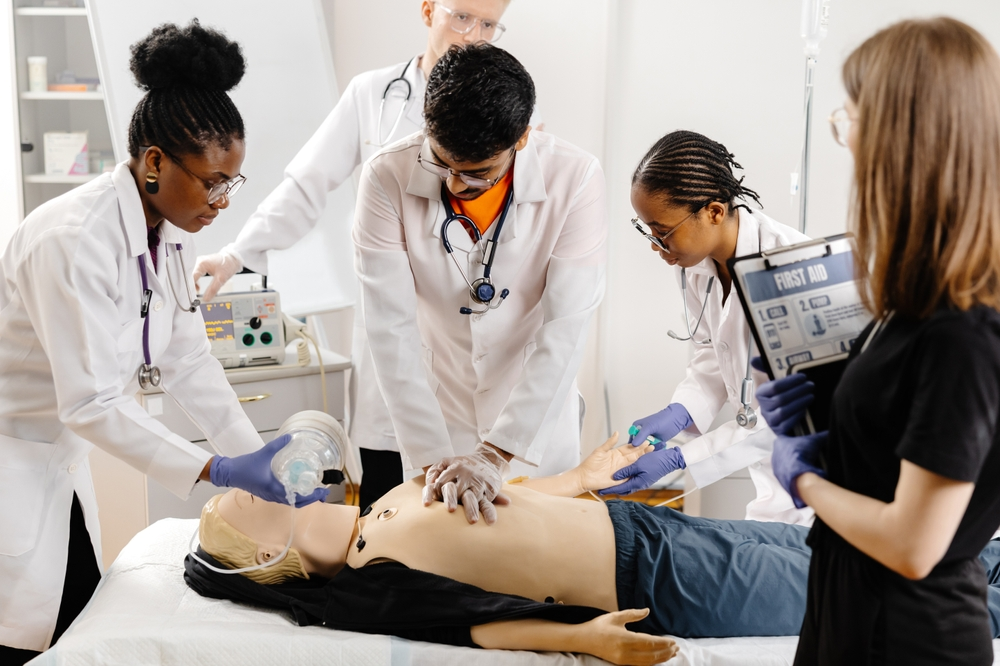
However, managing AFib isn't solely about medication. In some cases, emergency situations may arise such as post-cardiac arrest, which require immediate medical attention and specific protocols to follow. It's essential to be prepared for such scenarios by understanding the Post Cardiac Arrest Algorithm, which equips individuals with life-saving skills and expert guidance for critical situations.
Additionally, it's important to stay updated on guideline changes related to BLS certification and other relevant areas. This knowledge can significantly enhance your ability to manage AFib effectively and respond appropriately in emergencies.
AFib presents through distinct symptoms that signal disruptions in your heart's normal rhythm. You might experience:
Diagnosis typically involves several medical tests:
AFib affects how well your heart works, not just causing irregular rhythms. The upper chambers of your heart (atria) beat in a disorganized way, making it hard for blood to flow smoothly through the heart. This chaotic beating creates conditions where blood can pool and form clots, especially in a small pouch called the left atrial appendage.
The presence of blood clots significantly raises your stroke risk. Statistics show AFib patients face a 5 times higher risk of stroke compared to those without the condition. These clots can travel to the brain, blocking blood flow and causing a stroke.
Arrhythmia drugs play a crucial role in managing AFib by:
Different classes of heart arrhythmia drugs target specific aspects of AFib:
Your doctor selects appropriate medications based on:
In cases where AFib leads to severe symptoms like adult tachycardia, specific algorithms can be employed for effective management. It's crucial to understand these algorithms, such as those found in ACLS algorithms, which provide structured approaches to handle various cardiac emergencies.
Moreover, staying updated with the latest practices through recertification courses can be beneficial for healthcare professionals dealing with such conditions. Regular assessments through quizzes like this one on AFib can also enhance understanding and preparedness in managing atrial fibrillation effectively.
AFib medications fall into three distinct categories, each targeting specific aspects of the condition. Understanding these classifications helps patients grasp their treatment plan's structure and purpose.
These medications focus on managing your heart rate, keeping it within a target range of 60-100 beats per minute at rest.
Rhythm control drugs work to restore and maintain your heart's normal sinus rhythm. Your doctor might prescribe these if rate control medications haven't provided adequate symptom relief.
Blood thinners reduce your stroke risk by preventing clot formation in the heart's chambers.
Your healthcare provider will consider these factors when selecting the most appropriate medications for your situation:
The choice between rate control and rhythm control strategies depends on various factors, including:
Regular monitoring and adjustment of your medication regimen ensures optimal treatment outcomes while minimizing potential side effects.
In addition to understanding medication options, it's crucial for patients to be well-prepared for medical consultations. This includes being knowledgeable about best study tips for online course takers which can significantly enhance learning outcomes. For instance, mastering topics like solo provider adult BLS or post-resuscitation management transfer to tertiary care can provide valuable insights into patient care during AFib treatment.

Rate control medications serve as essential tools in AFib management by targeting the heart's electrical conduction system to slow rapid ventricular rates. These drugs help maintain heart rates within a target range of 60-100 beats per minute at rest.
Beta blockers work by blocking the effects of adrenaline and other stress hormones on the heart. These medications reduce heart rate and blood pressure by:
Common beta blockers prescribed for AFib include:
These medications prevent calcium from entering heart cells, resulting in:
Two main types are prescribed for AFib:
Digoxin (Lanoxin) represents a unique class of rate control medication that:
Patient-specific considerations:
Rate control drugs require careful dose adjustment based on:
For those interested in understanding more about the impact of these medications, you might want to consider taking some quizzes to test your knowledge or learn further about this subject.
Rhythm control therapy aims to restore and maintain your heart's normal sinus rhythm, reducing AFib episodes and improving quality of life. This strategy proves particularly beneficial for patients with persistent symptoms despite rate control.
Key Goals of Rhythm Control:
Common Drug Interactions:
Required Safety Monitoring:
Your doctor will select an appropriate antiarrhythmic based on:
AFib patients face a significant risk of stroke due to blood clot formation in the heart. These clots can travel to the brain, making anticoagulation therapy essential for stroke prevention. Studies show that proper anticoagulation reduces stroke risk by up to 70% in AFib patients1.
Warfarin (Coumadin) has been the standard anticoagulant for decades. While effective, it presents several challenges:
Modern anticoagulants offer improved convenience and safety profiles compared to warfarin:
Apixaban (Eliquis)
Dabigatran (Pradaxa)
Rivaroxaban (Xarelto)
Edoxaban (Savaysa)
Your healthcare provider will consider several factors when choosing an anticoagulant:
NOACs eliminate the need for regular INR testing but require:
Blood thinners carry a significant responsibility and understanding their effects is crucial. For instance, knowing how to handle potential emergencies related to AFib or its treatment can be lifesaving. This is where skills acquired from courses like PALS, which focus on handling pediatric emergencies, can be beneficial.
Successful AFib management hinges on proper medication administration. Studies show that patients who strictly follow their prescribed medication schedules experience better outcomes and fewer complications.
Digital drug checker tools help identify potential interactions between:
Popular drug checker resources include:
Certain medications require regular blood tests, some drugs need dose adjustments based on kidney function, and drug levels may be affected by diet changes. Travel across time zones requires careful medication timing planning.
In emergency situations, knowing basic life support (BLS) can be crucial. You can enhance your skills through online BLS certification courses.
For specific scenarios like pediatric emergencies, it's beneficial to understand the Pediatric Basic Life Support Algorithm, which outlines the foundational pathway for pediatric BLS when two or more rescuers are present. Additionally, being aware of common household hazards can aid in preventing accidents.
Proper medication administration requires attention to detail and consistent habits. Working closely with your healthcare team ensures you receive maximum benefit from your prescribed AFib treatment regimen.
Selecting the right AFib medications requires careful evaluation of multiple factors. Medical professionals assess medication effectiveness through specific criteria:
Key Effectiveness Markers:
The safety profile of AFib medications plays a crucial role in treatment success. Your healthcare provider will monitor:
Different medications work better for different patients. Your doctor will evaluate:
Your treatment plan might change based on:
In some cases, such as during a medical emergency where immediate care is needed, moving a patient may be necessary. However, this should generally be avoided unless there's a direct danger to the patient's life.
Regular assessment helps optimize your medication regimen:
Your healthcare team will work with you to find the most effective combination of medications that suits your specific needs while maintaining safety and improving outcomes.
AFib patients unresponsive to medications have access to effective non-pharmacological treatment options. These interventions can restore normal heart rhythm and reduce dependence on long-term medications.
Ideal for patients with:
Success rates: 60-80% of patients achieve normal rhythm
Recommended for:
Pre-procedure evaluation includes:
Recovery typically requires 48-72 hours
Regular follow-up monitoring ensures sustained benefits
Some patients may need repeat procedures for optimal results
These interventional approaches offer a path to improved heart rhythm control when medications alone prove insufficient. Your healthcare provider can determine if you're a suitable candidate based on your AFib pattern, age, and overall health status.
Leading a healthy lifestyle is just as important as taking medication when it comes to managing AFib effectively. The way you live your life can have a big impact on how well your treatment plan works.
Making smart choices about what you eat can help manage your AFib symptoms. Here are some dietary guidelines to follow:
Physical activity plays a key role in managing AFib. Here's how you can incorporate exercise into your routine:
Certain substances can worsen AFib symptoms or trigger episodes:
Getting enough sleep and managing stress are crucial for overall health. Here are some tips:
These lifestyle changes work hand in hand with the medications prescribed by your doctor to improve treatment results. It's important to keep an open line of communication with your healthcare provider so they can tailor these recommendations based on your individual needs and how you respond to treatment.
Successful AFib management requires vigilant tracking of your symptoms and medication responses. A dedicated symptom diary helps you record:
Your cardiology team needs these detailed observations to make informed decisions about your treatment plan. Many patients find mobile apps or smart devices helpful for logging this information systematically.
During these appointments, your healthcare provider will:
Blood pressure monitoring at home provides valuable data between visits. Keep a log of your readings, particularly when starting new medications or adjusting doses. This information helps your healthcare team identify patterns and optimize your treatment strategy.
Consider joining AFib support groups where you can share experiences and learn from others managing similar challenges. These communities often provide practical tips for tracking symptoms and maintaining medication schedules.
It's also essential to be aware of other potential health issues that could arise during AFib treatment, such as a heart attack. Recognizing the symptoms of a heart attack—like chest tightness, nausea, or shortness of breath—can be crucial. In such cases, it's important to call 911 immediately and be prepared to start CPR if necessary.
Furthermore, staying updated with the latest in emergency response techniques can greatly benefit both you and your healthcare team. Consider enrolling in an ACLS & BLS Recertification Bundle for Groups. This course not only covers essential life-saving techniques but also offers unlimited retakes if necessary at no charge, ensuring you're always prepared for any medical emergencies that may arise during your treatment journey.
Research in AFib medication development continues to advance, with promising new drugs in various stages of clinical trials. Scientists are focusing on creating treatments with enhanced safety profiles and improved effectiveness.
In parallel with these advancements, research teams worldwide are investigating natural compounds with antiarrhythmic properties. These substances could lead to new treatment options with fewer side effects than current medications. Clinical trials are also exploring combinations of existing drugs at lower doses to maintain effectiveness while reducing adverse reactions.
The development of these new medications represents a significant step toward more personalized and effective AFib treatment strategies. Ongoing studies continue to reveal promising candidates that could reshape the landscape of AFib therapy.
In the context of these advancements, it's crucial for healthcare professionals to stay updated on the latest ACLS algorithms which simplify emergency care training and improve life-saving skills effectively.
Managing AFib requires a proactive and personalized approach to achieve the best possible outcomes. Your journey with AFib medications needs dedication, awareness, and partnership with your healthcare team.
Key takeaways for successful AFib management:
The world of atrial drugs is constantly changing, offering better options for both controlling heart rate and preventing strokes. Your active involvement in treatment decisions, along with a clear understanding of your medications, sets the stage for successful AFib management.
Remember: AFib treatment isn't just about taking medications—it's about adopting a comprehensive approach to heart health. By staying informed about your condition, having regular medical check-ups, and making recommended lifestyle changes, you're taking important steps toward managing your AFib effectively.
Your commitment to following prescribed medication regimens, combined with healthy lifestyle choices, sets you up for the best possible outcomes in your AFib journey. Additionally, advancements like the impact of AI on emergency cardiac care are transforming how we manage these conditions by enhancing diagnosis accuracy and treatment precision.
.jpg)

