Pulmonary embolism (PE) is a life-threatening cardiovascular emergency that affects millions of people around the world and has high rates of illness and death. It happens when blood clots, usually from deep vein thrombosis, travel to the lungs and block the pulmonary arteries. The severity of PE can vary, with some cases showing no symptoms and others (called massive PE) requiring immediate treatment due to a drop in blood pressure.
Shock in massive pulmonary embolism occurs when large clots block blood flow to the lungs, causing a series of physiological changes. The right ventricle has to work harder against increased resistance, leading to strain on the heart, reduced blood flow, and low blood pressure. If this condition is not recognized and treated quickly, it can lead to complete failure of the cardiovascular system.
In such situations, it becomes crucial for healthcare providers to master advanced life support techniques. They should consider enrolling in an ACLS & BLS Recertification Bundle for Groups, which includes essential courses such as ER Physician written course and offers unlimited retakes if necessary at no charge.
The diagnostic challenge becomes even greater when patients with massive PE show ST-segment elevation on their electrocardiogram (ECG). This finding is usually associated with a heart attack but can also appear during severe episodes of pulmonary embolism. The ST elevation on the ECG indicates ischemia (lack of blood flow) to the right ventricle instead of blockage in the coronary arteries, creating a difficult situation that can delay proper treatment.
It is important for healthcare providers to understand how shock, ST-segment elevation, and massive pulmonary embolism are connected so they can tell this condition apart from acute coronary syndromes (heart attacks) and start life-saving interventions. In critical situations like these, following a structured Post Cardiac Arrest Algorithm can help manage these complex cases effectively. Additionally, healthcare professionals should regularly take relevant quizzes like those found in lesson 4 and lesson 19 review sections on ACLS certification websites to stay updated with the latest protocols.
Pulmonary embolism is a serious condition where blood clots block the flow of blood in the lungs, potentially leading to a life-threatening situation. These clots usually form in the deep veins of the legs and can travel to the lungs, causing various physiological problems that may quickly result in cardiovascular failure.
The development of pulmonary embolism follows a predictable pathway that starts with deep venous thrombosis (DVT). Clots form within the deep veins of the legs, pelvis, or arms due to Virchow's triad: venous stasis, endothelial injury, and hypercoagulability. These thrombi can remain stable for extended periods, but mechanical forces such as sudden movement, coughing, or changes in venous pressure can dislodge fragments.
Once these clot fragments are released, they travel through the veins and enter the right side of the heart before reaching the pulmonary artery, which supplies blood to the lungs. The impact of this blockage depends on the size and quantity of the clots. Larger clots may become trapped in the main pulmonary arteries or their major branches, while smaller fragments can obstruct smaller blood vessels throughout the lung tissue.
When a clot blocks a pulmonary artery, it creates an immediate obstacle to blood flow. This forces the right ventricle of the heart to work harder and generate higher pressures in order to maintain adequate blood circulation. As a result, there is an acute increase in resistance within the pulmonary blood vessels, leading to strain on the right side of the heart and potentially causing right ventricular failure.
Additionally, this obstruction reduces the effective area available for blood flow in the lungs, resulting in mismatches between ventilation (airflow) and perfusion (blood flow) that hinder oxygen exchange. In severe cases, increased pressure in the pulmonary capillaries may lead to fluid accumulation in the lungs (pulmonary edema), although this mechanism differs from edema caused by left-sided heart failure.
Certain factors increase the likelihood of developing venous thromboembolism (VTE), which includes both DVT and PE:
Given how serious conditions like PE and DVT can be, it's important to be ready for emergencies. Taking courses such as PALS can improve your abilities and make sure you're prepared to effectively manage any situation that arises.
Shock is the most severe form of massive pulmonary embolism, occurring when more than 50% of the pulmonary arteries are blocked. This life-threatening condition causes hemodynamic instability, which is indicated by a systolic blood pressure below 90 mmHg or a drop of at least 40 mmHg from the usual level for over 15 minutes. You can identify shock in massive PE through clinical signs such as confusion, cold hands and feet, decreased urine output, and high lactate levels showing poor blood flow to the tissues.
Shock follows a predictable pattern of events in the cardiovascular system. When there is a large blockage in the lungs, it creates immediate resistance in the blood vessels, making it harder for blood to flow through. As a result, the right side of the heart has to work much harder to pump blood into the lungs.
In this situation, the right ventricle (the chamber of the heart that pumps blood to the lungs) experiences a sudden increase in pressure. This causes the right ventricle to stretch and enlarge as it tries to maintain its pumping ability. However, this enlargement also affects the left ventricle (the chamber of the heart that pumps blood to the rest of the body) because both ventricles are interconnected. The enlarged right ventricle pushes against the wall separating them (the interventricular septum), making it difficult for the left ventricle to fill properly.
As a result, there is less blood being pumped out by the left ventricle, leading to lower blood pressure and inadequate blood supply to vital organs.
The enlarged right ventricle faces a critical problem where its need for oxygen exceeds what it can supply. The demand for oxygen increases significantly due to higher tension on its walls and an increased heart rate as compensatory mechanisms kick in to maintain blood flow. At the same time, systemic low blood pressure reduces blood flow to the coronary arteries that supply oxygen-rich blood directly into this chamber.
This imbalance between supply and demand creates a condition known as right ventricular ischemia, which can be detected by elevated levels of troponin (a marker for heart damage) in many patients with massive PE. The ischemic right ventricle becomes increasingly weak and unable to contract effectively, leading to further enlargement and increased need for oxygen.
You may notice worsening tricuspid regurgitation (backward flow of blood from right ventricle into right atrium) and elevated jugular venous pressure (indicating increased pressure in veins returning blood from body).
In such critical situations, understanding adult chain of survival is crucial. This knowledge can guide healthcare providers in implementing effective interventions during emergencies like massive pulmonary embolism.
Furthermore, BLS certification plays an essential role in preparing individuals to respond adequately in such medical emergencies. The training includes vital sections that condense essential information into manageable parts for easier understanding and retention.
To reinforce learning and assess comprehension of these critical topics, engaging with quizzes related to BLS certification can be beneficial. These quizzes serve as an effective tool for reviewing important concepts and ensuring readiness for real-life applications of this knowledge.
In addition to BLS training, it's also important to have knowledge about specific conditions such as stroke, which may present similarly to massive pulmonary embolism but require different management strategies. Understanding these nuances can significantly enhance patient outcomes during emergency situations.
The electrocardiogram serves as a crucial diagnostic tool in pulmonary embolism cases, though ECG changes can range from subtle abnormalities to dramatic findings that mimic other cardiac conditions. You'll encounter varying degrees of electrical disturbances depending on the severity and extent of the pulmonary vascular obstruction.
These findings collectively paint a picture of acute right heart stress that distinguishes pulmonary embolism from left-sided cardiac pathology.
In such critical situations where immediate medical intervention is required, having advanced knowledge and skills can make a significant difference. For healthcare professionals dealing with pediatric patients, PALS certification could prove invaluable. This certification equips them with essential skills needed to manage emergencies such as sudden cardiac arrest or severe allergic reactions in children.
Moreover, for those seeking to enhance their life-saving skills further, ACLS algorithms provide concise and easy-to-follow guidelines designed to simplify emergency care training.
Lastly, if you're preparing for certification exams such as BLS or ACLS, it's crucial to have effective study strategies. Implementing best study tips tailored for online course takers can greatly enhance your learning experience and success rate.
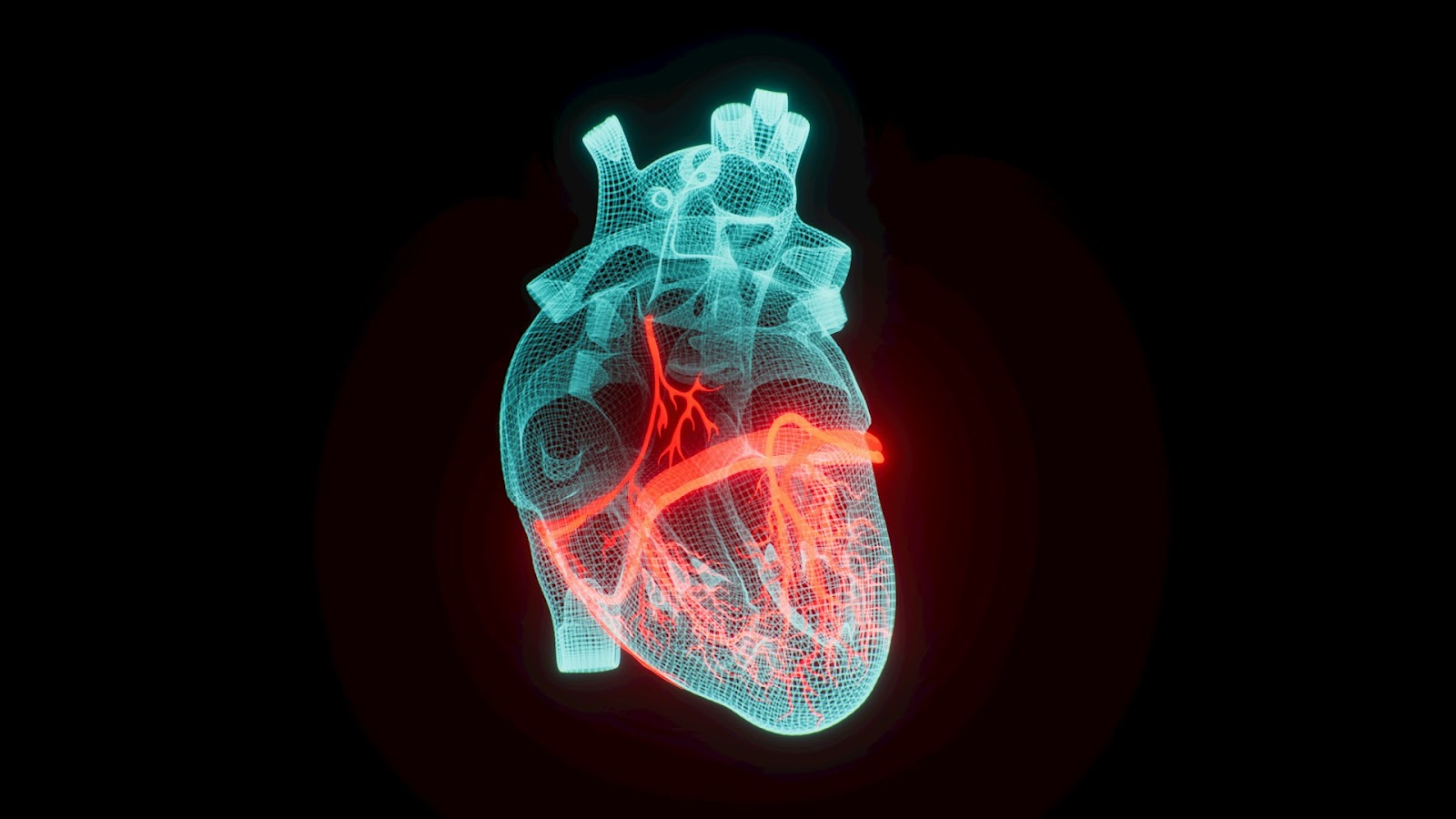
ST-segment elevation is one of the most difficult ECG findings in massive pulmonary embolism. It can be confusing to diagnose because it looks very similar to an acute myocardial infarction (heart attack). This type of ECG ST elevation happens in about 10-15% of severe PE cases, mostly showing up in specific lead areas that reflect the underlying disease process.
The st segment elevation in massive PE usually shows up in two main ways:
In massive PE, right ventricular ischemia causes the development of st wave elevation. When there is a sudden increase in resistance in the blood vessels of the lungs, the right ventricle has to work harder and generate higher pressures. This creates a mismatch between the supply and demand for blood flow, leading to strain on the heart.
The electrical changes caused by this strain can look very similar to those seen in blockages of the coronary arteries. That's why it's easy to mistake this condition for a heart attack when looking at an ECG for the first time.
It's important to note that when the right side of the heart is not getting enough blood flow, it can also affect other parts of the body. You may see signs such as elevated pressure in the veins of the neck (jugular venous pressure) or abnormal sounds when listening to the heart (tricuspid regurgitation murmurs). These additional clues can help doctors interpret the ECG more accurately.
In complex situations where a patient needs special care after being revived from cardiac arrest, it's crucial to have a clear plan. For example, when transferring a patient to a higher-level hospital for further treatment, all relevant medical information and history should be communicated smoothly between healthcare providers. This ensures that the patient receives continuous and optimal care throughout their journey.
When ST-segment elevation appears on ECG, it's crucial to differentiate between massive pulmonary embolism (PE) and ST-segment elevation myocardial infarction (STEMI). Both conditions are medical emergencies that require immediate intervention, but the treatments are different. Here are some key clinical features that can help you determine whether it's PE or acute myocardial infarction.
Respiratory symptoms are often the most telling signs. Patients with massive PE usually have low oxygen levels (hypoxia) but normal lung sounds when examined. In contrast, isolated STEMI patients often have normal oxygen saturation levels. Another clue is low levels of end-tidal carbon dioxide (end-tidal CO2), which indicates increased dead space ventilation—a characteristic of pulmonary embolism.
Evaluating risk factors is also important in your clinical assessment. Consider the following:
It's noteworthy that perioperative pulmonary embolism can occur in patients undergoing surgery, making it crucial to assess these factors thoroughly.
Echocardiography can be a valuable diagnostic tool in this case. It can show signs of right ventricular dysfunction such as enlargement, decreased movement, and high pressures in the pulmonary artery. These findings are different from what you would typically see in STEMI, where there are abnormalities in the movement of the left ventricle wall.
By combining respiratory symptoms, relevant risk factors, and echocardiographic evidence of strain on the right side of the heart, you can create a strong clinical picture that helps differentiate between massive PE and blocked coronary arteries—even when ST-segment elevation makes interpreting the electrocardiogram more challenging.
The differential diagnosis between massive pulmonary embolism and acute myocardial infarction becomes particularly complex when both conditions present with shock and ST-segment elevation. You need to recognize that these overlapping presentations can lead to critical delays in appropriate treatment.
In such scenarios, especially when dealing with pediatric patients, having a clear understanding of the Pediatric Basic Life Support Algorithm – 2 Rescuers is essential. This algorithm serves as the foundational pathway for pediatric BLS when 2 or more rescuers are present. It includes vital steps such as scene safety, compressions, ventilation, and AED use.
Echocardiography serves as your most valuable diagnostic tool for identifying right ventricular dysfunction. When you perform bedside echocardiography, look for specific patterns that distinguish massive pulmonary embolism from AMI:
You'll find that patients with massive PE typically demonstrate hypoxia with clear lungs on chest examination, contrasting with the pulmonary edema often seen in cardiogenic shock from AMI. Monitor end-tidal CO2 levels, as they remain characteristically low in PE due to increased dead space ventilation from impaired pulmonary perfusion.
The echocardiographic findings of right heart strain, combined with preserved left ventricular systolic function, strongly support PE as the underlying cause of shock. You can use these imaging findings to guide your treatment decisions rapidly, especially when CT angiography isn't immediately available or when the patient's hemodynamic status is too unstable for transport.
The symptoms of a PE that progresses to shock present as a combination of respiratory, cardiovascular, and neurological signs that require immediate recognition. Here are the key symptoms to look out for:
As the body tries to compensate for the drop in blood flow, certain vital signs will change:
These symptoms create a picture of acute failure in both the heart and lungs. Patients will show signs of poor blood flow such as cool limbs, delayed capillary refill, and confusion. The combination of breathing distress with unstable blood flow is an emergency that needs immediate action to prevent heart failure and death.
In these situations, it's generally not advised to move someone unless their life is directly at risk or if you need to provide care. But if movement is necessary, make sure you use proper techniques like putting an unconscious victim who is breathing and has a pulse into the recovery position to protect their airway and reduce the risk of choking.
Time is tissue when managing massive PE complicated by shock. The primary goals focus on immediate hemodynamic stabilization, restoration of pulmonary blood flow, and prevention of cardiovascular collapse. You must act swiftly as mortality rates exceed 30% without prompt intervention.
Treatment for PE begins with aggressive supportive care:
Thrombolysis represents the cornerstone of PE medical treatment for hemodynamically unstable patients. You should consider systemic thrombolysis when:
Standard thrombolytic protocols include:
When thrombolysis fails or contraindications exist, surgical intervention becomes necessary:
You must weigh bleeding risks against potential mortality. Major bleeding occurs in 6-20% of patients receiving systemic thrombolysis, yet untreated massive PE carries significantly higher mortality risk. Age over 75, recent surgery, and active bleeding represent relative contraindications requiring individualized decision-making.
Success depends on rapid implementation of appropriate strategies tailored to each patient's unique circumstances.
ECG ST segment elevation monitoring becomes crucial once treatment for PE begins, as you need to track the dynamic response to therapeutic interventions. Continuous cardiac monitoring allows you to assess whether your patient's condition is improving or deteriorating in real-time.
When administering thrombolytic therapy, you should expect to see gradual resolution of ST changes as right ventricular strain decreases. The ST-segment elevation in leads V1-V3 typically begins to normalize within hours of successful reperfusion. This improvement serves as an early indicator that your treatment is working effectively.
QRS segment changes provide additional prognostic information during treatment monitoring:
The speed at which QRS segment abnormalities resolve directly correlates with patient outcomes in Massive Pulmonary Embolism. You should document:
Persistent ST changes beyond 12 hours may indicate incomplete clot resolution or ongoing right heart dysfunction. These patients often require escalation to more aggressive interventions like catheter-directed therapy or surgical embolectomy.
Your ECG monitoring strategy should integrate with hemodynamic parameters and echocardiographic findings. When ST-Segment Elevation resolves alongside improving blood pressure and oxygen saturation, you can be confident that your treatment for PE is achieving its therapeutic goals. The QRS segment changes serve as a roadmap for assessing the extent of right ventricular recovery during the critical treatment phase.
Early diagnosis is crucial when managing patients with shock and ST-segment elevation due to massive pulmonary embolism. Quick decision-making can directly affect patient survival rates, as delayed recognition can be fatal within hours.
Differentiating between acute myocardial infarction and massive PE can be challenging. It's important to stay vigilant and consider the following factors when patients present with:
However, the prognosis of massive pulmonary embolism improves significantly when targeted treatment strategies are implemented promptly. Thrombolytic therapy, when indicated and given early, can reverse the hemodynamic collapse and prevent progression to cardiac arrest.
Continuous ECG monitoring allows you to assess the patient's changing cardiovascular status during treatment. You'll notice fluctuations in both ST-segment elevation and QRS morphology that indicate the effectiveness of your interventions and inform ongoing management choices.
The key to better outcomes lies in your ability to quickly recognize the combination of findings - shock, ST-segment elevation, and massive pulmonary embolism - and start appropriate treatment without delay. This systematic approach turns a potentially deadly condition into a manageable emergency with better chances of survival.
Additionally, using technology like AI can greatly improve these outcomes. The impact of AI on emergency cardiac care is significant, as it enhances diagnosis, treatment accuracy, and patient results through advanced data analysis and real-time decision support.
.jpg)

