Pediatric emergencies demand swift, precise interventions to save lives and optimize outcomes. Healthcare professionals face the immense responsibility of being prepared to manage these critical situations effectively. Acquiring the knowledge and skills necessary to navigate the complexities of pediatric resuscitation is paramount.
Pediatric Advanced Cardiovascular Life Support (ACLS) and Pediatric Advanced Life Support (PALS) are two essential training programs designed to equip healthcare providers with the expertise needed to respond to life-threatening events in infants and children. While both courses share the common goal of improving pediatric resuscitation, they differ in their focus and target audience.
In this comprehensive guide, we will delve into the key differences between Pediatric ACLS and PALS, explore the core components of each training program, and provide valuable insights to help healthcare professionals enhance their skills in managing pediatric emergencies.
What is Pediatric Advanced Cardiovascular Life Support (ACLS)?
Pediatric ACLS is a specialized resuscitation training program that focuses on advanced interventions for infants and children experiencing cardiopulmonary emergencies. Building upon the foundation of pediatric basic life support (BLS) skills, Pediatric ACLS equips healthcare providers with the knowledge and techniques necessary to recognize and manage life-threatening conditions in the pediatric population.
The key components of Pediatric ACLS include:
- Advanced Airway Management: Pediatric ACLS training emphasizes the unique challenges of managing the airway in infants and children. Participants learn techniques for effective ventilation, intubation, and the use of advanced airway devices specifically designed for pediatric patients.
- Vascular Access: Obtaining vascular access in pediatric patients can be challenging due to their smaller size and anatomical differences. Pediatric ACLS covers various techniques for establishing intravenous or intraosseous access, ensuring timely administration of medications and fluids during resuscitation efforts.
- Medication Administration: The course provides comprehensive guidance on pediatric ACLS medications, including their indications, dosages, and routes of administration. Healthcare providers learn to calculate weight-based doses accurately and deliver medications safely in high-stress situations.
- Resuscitation Algorithms: Pediatric ACLS training focuses on resuscitation algorithms tailored to the specific needs of infants and children. These algorithms guide healthcare providers through the systematic assessment and management of cardiac arrest, symptomatic bradycardia, and other cardiopulmonary emergencies.
- Post-Resuscitation Care: Effective post-resuscitation care is crucial for optimizing patient outcomes. Pediatric ACLS covers the stabilization and ongoing management of pediatric patients following successful resuscitation, including targeted temperature management, hemodynamic support, and neuroprotective strategies.
By mastering these key components, healthcare providers gain the confidence and expertise necessary to deliver high-quality resuscitation care to critically ill infants and children. Pediatric ACLS certification, like we offer at Affordable ACLS, demonstrates a commitment to excellence in pediatric emergency care and ensures that healthcare professionals are prepared to make a difference when every second counts.
What is Pediatric Advanced Life Support (PALS)?
Pediatric Advanced Life Support (PALS) is a critical training program designed to provide healthcare professionals with the expertise needed to manage emergencies in infants and children. This specialized course focuses on equipping providers with the skills required for timely and effective interventions during acute pediatric crises.
Core Components of PALS
PALS emphasizes a structured method for assessing pediatric patients, known as the pediatric assessment triangle. This approach allows healthcare providers to quickly evaluate a child’s condition by observing their appearance, breathing effort, and circulation, facilitating rapid decision-making in emergency situations.
- Respiratory Emergencies: The course covers the identification and treatment of various respiratory issues, stressing the importance of immediate intervention to prevent progression to life-threatening conditions. Techniques such as airway stabilization and supplemental oxygen delivery are integral parts of the training.
- Shock States: PALS addresses the recognition and management of different shock types, including hypovolemic and distributive shock. Trainees learn to detect early indicators and implement interventions that restore effective circulation and prevent organ failure.
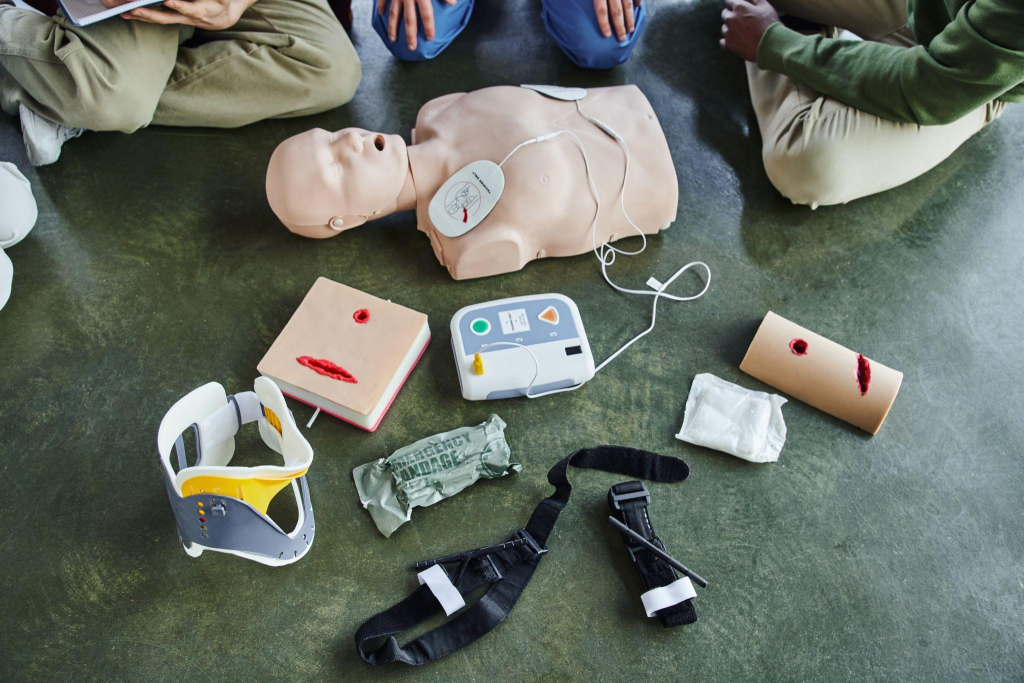
- Cardiopulmonary Arrest: Detailed protocols for managing cardiac arrest in children are a key component of PALS. The course includes training on performing effective chest compressions, appropriate ventilation, and the application of pediatric defibrillation when indicated.
Key Differences Between PALS and ACLS
PALS and ACLS target different patient demographics and medical conditions. PALS is specifically oriented towards pediatric emergencies, focusing on early intervention for respiratory and circulatory issues, whereas ACLS is more centered on adult cardiac emergencies.
- Medication Dosing: PALS requires individualized medication dosing based on the child’s weight and age, necessitating precise calculations for safe and effective administration. This tailored approach contrasts with the more standardized dosing often seen in ACLS.
- Pediatric-Specific Assessment: PALS provides comprehensive training on pediatric assessment, emphasizing early detection of clinical deterioration. This equips providers with the ability to respond quickly to prevent further decline, ensuring timely intervention that is crucial in pediatric care.
Through PALS training, healthcare providers develop the competencies necessary to deliver exceptional emergency care to children, enhancing their ability to respond effectively to pediatric health crises.
The Importance of Pediatric ACLS and PALS Training

Training in Pediatric ACLS and PALS equips healthcare professionals with crucial competencies for managing pediatric emergencies. These programs prepare providers to address the distinctive challenges posed by critically ill infants and children, fostering a readiness to act decisively under pressure. By focusing on pediatric-specific needs, these courses enable practitioners to deliver precise and effective interventions, enhancing patient safety and outcomes.
Excellence in Pediatric Emergency Care
Delivering exceptional pediatric emergency care is a primary goal of Pediatric ACLS and PALS training. Providers learn to execute interventions with accuracy, whether through advanced airway techniques or precise medication administration. This focus on detail ensures that care is responsive to the unique physiology of pediatric patients, promoting better survival rates and neurological health.
- Structured Assessment: The training emphasizes a methodical approach to evaluating and managing emergencies, facilitating rapid identification and treatment of critical conditions. This structured assessment helps minimize response times and improves the effectiveness of care.
- Collaborative Teamwork: Functioning as an integrated team is essential during pediatric resuscitations. Both courses highlight the importance of teamwork, including effective communication and coordinated efforts, which are critical for achieving successful outcomes.
Healthcare Providers Who Benefit from Pediatric ACLS Certification
Pediatric ACLS certification significantly enhances the capabilities of healthcare professionals across various environments. It not only improves individual proficiency but also elevates the overall standard of care within medical teams.
- Emergency Department Personnel: These professionals often encounter pediatric emergencies first and must be skilled in initiating and managing resuscitation efforts efficiently.
- Staff in Pediatric and Neonatal Intensive Care Units: In these settings, caregivers deal with complex cases involving critically ill children, necessitating up-to-date skills and knowledge for effective intervention.
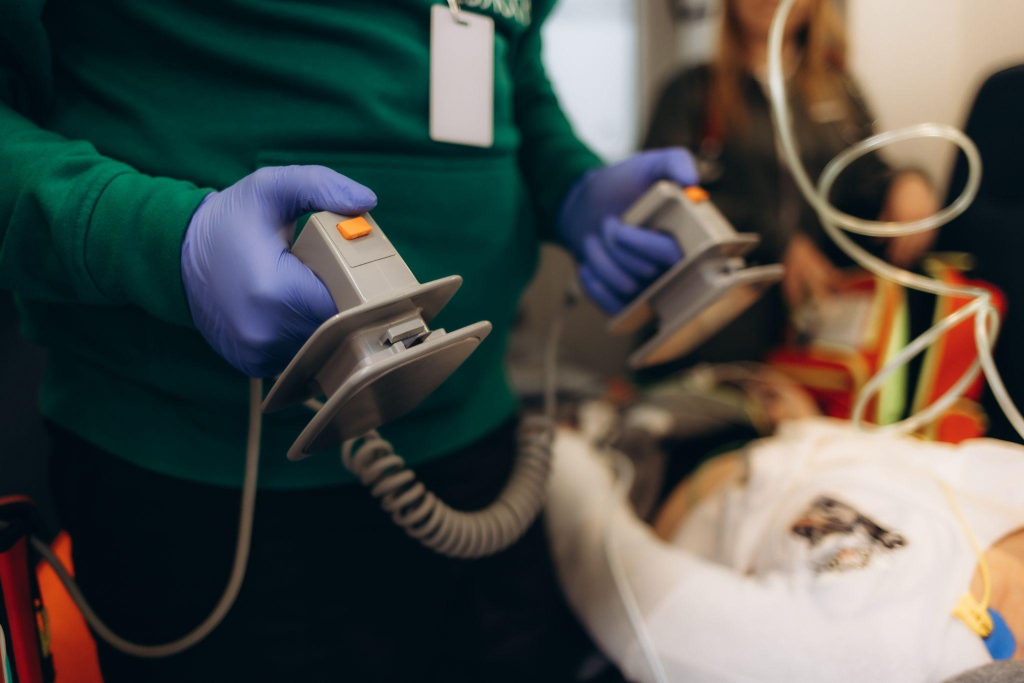
- EMS and Critical Care Transport Teams: These teams play a vital role in stabilizing and transporting pediatric patients, requiring comprehensive understanding of pediatric protocols to ensure safe care during transit.
- Inpatient Pediatric Healthcare Providers: In hospital settings, these providers must be adept at recognizing and responding to signs of deterioration in pediatric patients, making certification essential for maintaining high-quality patient care.
Through Pediatric ACLS and PALS training, healthcare providers are equipped with the skills necessary to address the complexities of pediatric emergencies, ultimately improving care delivery and patient outcomes.
Implementing Pediatric ACLS and PALS Principles

Effectively implementing Pediatric ACLS and PALS principles requires healthcare providers to remain acutely aware of any signs of distress in pediatric patients. Early recognition of potential complications allows for immediate interventions, which are crucial in altering the course of an emergency. Swift and precise assessment leads to informed decision-making during critical moments.
The cornerstone of pediatric resuscitation is prompt action, specifically in delivering effective interventions. Initiating life-saving measures, such as manual ventilation and ensuring adequate oxygenation, is vital to address respiratory compromise swiftly. The execution of well-defined protocols ensures that each intervention aligns with best practices, facilitating a seamless approach to pediatric care. Team coordination is vital—clear roles and efficient communication enhance the synergy needed for successful outcomes.
Following resuscitation efforts, attention shifts to stabilizing the patient. This involves not only managing physiological parameters but also preparing for potential complications. Ensuring a smooth transition to intensive care settings is key, where ongoing monitoring and tailored interventions can continue to support recovery. This phase requires a comprehensive understanding of pediatric pathophysiology to inform the best course of action for each unique case.
Overcoming Challenges in Pediatric Resuscitation
Pediatric resuscitation presents distinct challenges that differ significantly from adult care. The anatomical nuances of pediatric airways necessitate specialized techniques for maintaining patency and ensuring effective ventilation. Vascular access, often more complex in children, demands proficiency in pediatric-specific approaches to ensure timely and effective treatment delivery.
Administering medications in pediatric emergencies requires meticulous attention to detail. Accurate dosing, tailored to the child’s weight and clinical scenario, is critical to achieving the desired therapeutic effect without adverse outcomes. This precision underscores the need for continuous training and familiarity with pediatric pharmacology.
Beyond the technical challenges, the emotional dimension of pediatric resuscitation cannot be overlooked. Providing support to families during these intense situations is imperative. Engaging families in the care process, offering clear explanations, and maintaining empathy throughout fosters a supportive environment. This approach not only aids in managing the immediate crisis but also contributes to the overall well-being of the patient and family.
Mastering the intricacies of Pediatric ACLS and PALS is a critical responsibility for healthcare professionals committed to delivering exceptional care to infants and children in life-threatening situations. By investing in comprehensive training and staying updated with the latest guidelines, you can make a profound difference in the lives of your pediatric patients and their families. We invite you to join us in our mission to advance pediatric resuscitation skills and knowledge by exploring our online certification and recertification courses designed to empower healthcare providers like you.