The integration of telemedicine into healthcare training has become increasingly relevant in today’s digital age. As technology advances, it opens up new possibilities for enhancing medical education and expanding access to life-saving skills.
One area where telemedicine holds significant potential is in Advanced Cardiovascular Life Support (ACLS) training. By leveraging digital communication tools, ACLS training programs can bridge geographical gaps and offer high-quality instruction to healthcare professionals in underserved areas.
However, effectively integrating telemedicine into ACLS training requires careful consideration of both the applications, challenges, and opportunities of telemedicine and the benefits involved. It necessitates a thorough understanding of the technological requirements, curriculum adaptations, and potential obstacles that may arise during implementation.
Why Integrate Telemedicine into ACLS Training?
Integrating telemedicine into ACLS training offers numerous advantages that can significantly enhance the learning experience and expand access to critical life-saving skills. By leveraging digital communication tools, ACLS training programs can overcome geographical barriers and reach healthcare professionals in underserved areas—a key benefit of telemedicine in healthcare.
Telehealth training allows participants to engage in ACLS courses remotely, eliminating the need for travel and reducing associated costs, showcasing the diverse applications of telemedicine in healthcare. This increased accessibility is particularly valuable for healthcare providers in rural or remote locations who may otherwise struggle to attend in-person training sessions. Furthermore, telemedicine integration enables a more flexible learning approach, allowing trainees to access course materials and participate in virtual simulations at their convenience.
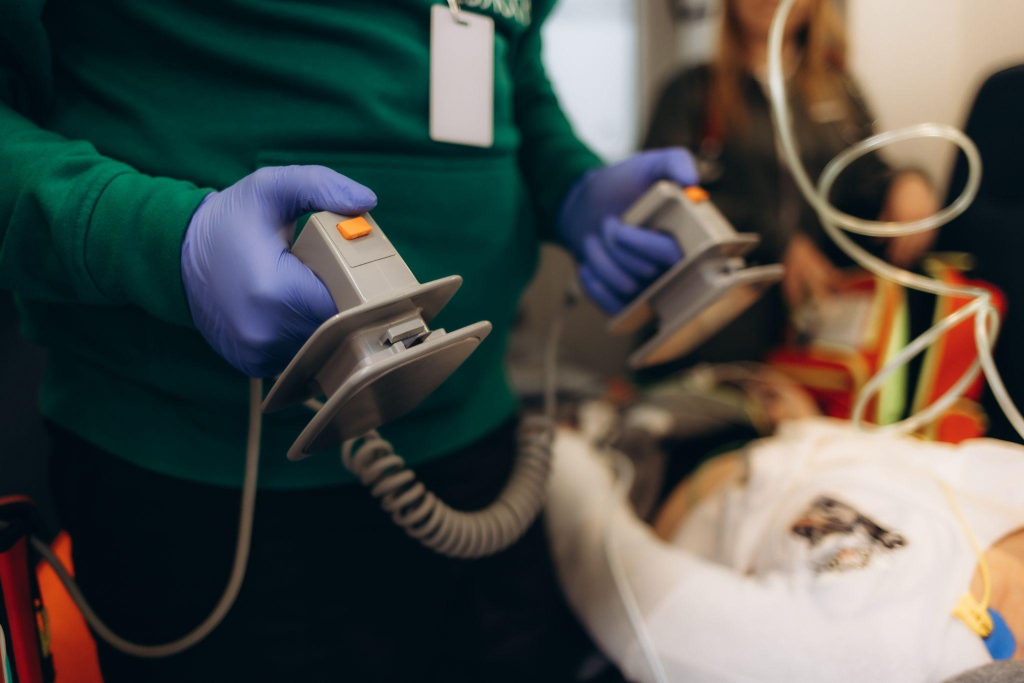
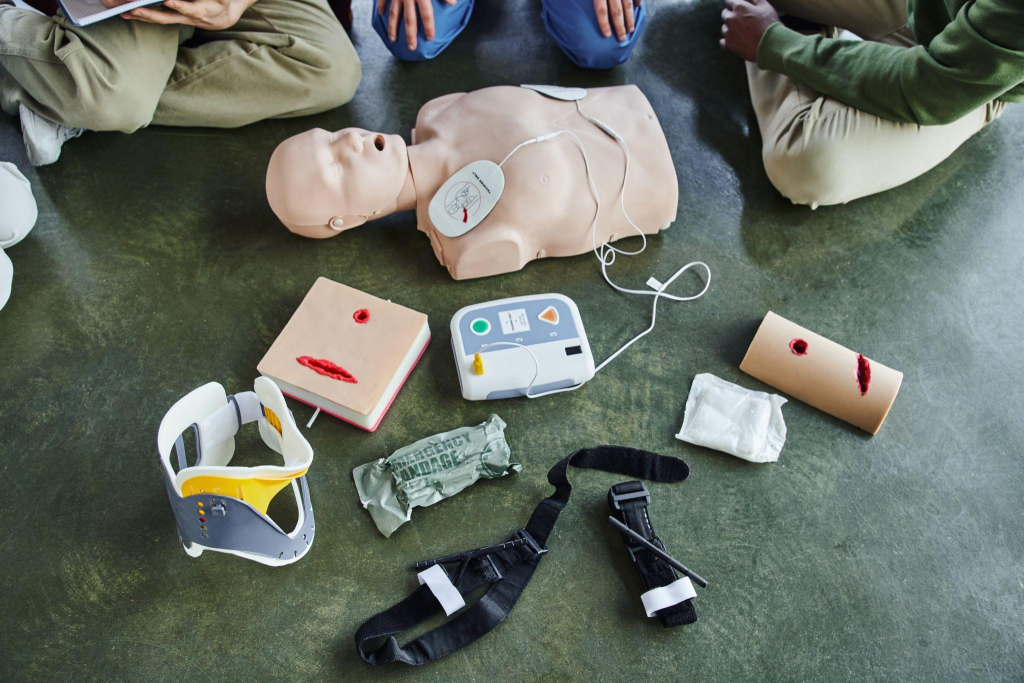
In addition to improving accessibility, integrating telemedicine into ACLS training can enhance learning outcomes. Virtual reality tools and tele-simulation platforms, such as those offered by Affordable ACLS, provide immersive experiences that closely mimic real-life ACLS scenarios. These technologies allow trainees to practice their skills in a safe and controlled environment, receiving immediate feedback and guidance from experienced instructors. By offering repeated practice opportunities and personalized coaching, telemedicine-based ACLS training can help healthcare professionals develop greater confidence and proficiency in applying life-saving techniques.
How to Integrate Telemedicine into ACLS Training

Successfully incorporating telemedicine into ACLS training requires a carefully crafted strategy that embraces both technological advancements and educational innovations. This process begins by evaluating the current technological landscape and making the necessary enhancements to accommodate telemedicine platforms. Aligning with digital health standards is vital for ensuring a cohesive integration that enriches the educational experience for healthcare practitioners.
Step 1: Evaluate Technological Infrastructure
The first step in implementing telemedicine effectively is a comprehensive analysis of existing technological resources. This includes assessing the infrastructure for internet quality, device capabilities, and software compatibility. Upgrades may be necessary to support robust video conferencing capabilities and interactive learning modules. Ensuring interoperability with current digital health solutions, such as secure telecommunication systems and electronic health records, is crucial for a smooth transition and aligns with the evaluation of telemedicine in healthcare delivery.
Step 2: Design an Enriched Curriculum
Creating a robust curriculum is central to integrating telemedicine into ACLS training. This involves incorporating advanced simulation tools and virtual reality technology to accurately represent clinical scenarios encountered in ACLS. By crafting courses that blend theoretical insights with practical telemedicine applications, trainees receive a holistic education, which can also highlight the impact of telemedicine on chronic disease management. Interactive elements should allow for adaptive feedback and scenario-based learning, equipping healthcare professionals with the skills needed for real-world emergencies.
Step 3: Prepare Educators and Facilitators
Equipping educators with the necessary skills to use telemedicine platforms effectively is essential for delivering high-quality instruction. Instructors need to be proficient in utilizing digital tools to foster interactive and engaging learning environments. Training sessions should focus on enhancing educators’ ability to deliver dynamic virtual training. By empowering educators with comprehensive knowledge and technical expertise, the integrity and effectiveness of ACLS training are upheld, ensuring healthcare providers are well-prepared for contemporary clinical demands.
Step 1: Assess Technological Needs
Integrating telemedicine into ACLS training requires a detailed examination of the current technological setup. This process involves pinpointing deficiencies and identifying opportunities to enhance systems for supporting telemedicine applications. Reliable network connections, up-to-date hardware, and compatible software form the backbone of any successful telemedicine integration, as outlined in telehealth application domains and technologies.
Ensuring that telemedicine solutions are in line with contemporary digital health standards is crucial. This alignment guarantees that telemedicine platforms function effectively and can integrate seamlessly with existing healthcare infrastructure. Selection of telemedicine tools should prioritize secure data exchange capabilities and interoperability with electronic health systems, thereby enhancing the training experience.
After the initial assessment, focus should transition to the implementation of necessary technological enhancements. Investment in state-of-the-art video conferencing capabilities, immersive simulation technologies, and robust communication networks is essential. These enhancements not only improve the delivery quality of telemedicine but also ensure that trainees have a consistent and enriching learning journey. By establishing technological readiness, ACLS training programs can fully capitalize on telemedicine, equipping healthcare professionals with the expertise required for critical interventions.
Step 2: Develop a Comprehensive Curriculum
Designing an effective curriculum for integrating telemedicine into ACLS training involves harnessing innovative educational strategies and advanced technology. The aim is to create engaging learning experiences that simulate the complexities of actual cardiac emergencies. By utilizing cutting-edge digital tools, trainees can explore a diverse range of scenarios in a virtual setting.
Utilize Advanced Simulation Techniques
To achieve this, the curriculum should leverage advanced simulation technologies that enable healthcare professionals to interact with realistic scenarios. These tools can emulate a variety of clinical environments, from hospital settings to remote locations. Through the use of interactive technology, trainees can practice critical interventions, such as advanced airway management or emergency pharmacology, in a safe context. This approach not only bolsters skill proficiency but also enhances situational awareness.
Structuring a Dynamic Course Framework
Beyond practical simulations, a well-rounded curriculum must integrate theoretical aspects that provide a comprehensive understanding of ACLS. This includes modules on the latest clinical guidelines, relevant pharmacology, and the physiological basis of cardiac emergencies. By embedding telemedicine applications within the course, such as virtual patient assessments and digital case reviews, trainees gain insights into the practical application of these technologies in clinical settings.
Course design should prioritize flexibility, allowing educators to adapt content to meet the specific needs of their audience. This could involve incorporating interactive discussions, multimedia resources, and collaborative problem-solving exercises that foster critical thinking and engagement. By creating a dynamic and adaptable learning environment, the curriculum ensures that healthcare professionals are thoroughly prepared with the theoretical knowledge and practical skills required for effective ACLS, tailored to the telemedicine context.
Step 3: Train Educators and Facilitators
The successful integration of telemedicine into ACLS training hinges on equipping educators with the skills and confidence needed to utilize digital platforms effectively. Educators must not only understand the intricacies of ACLS protocols but also possess the ability to navigate and optimize the use of telemedicine tools for educational purposes. Establishing a structured training program is essential to achieve this dual competency.
Building Technical Acumen in Educators
Training should commence with a focus on strengthening educators’ technical abilities to manage telemedicine systems efficiently. This includes interactive workshops that explore the functionalities of telemedicine platforms, address common technical challenges, and demonstrate the integration of virtual simulation tools. Through this hands-on approach, educators can develop the expertise necessary to facilitate seamless and effective training sessions, ensuring minimal disruptions.
Adapting Instructional Methods for Virtual Learning
Beyond mastering technology, educators need to adapt their teaching strategies to suit the unique demands of virtual learning environments. This involves employing innovative methods to engage learners, such as utilizing digital storytelling, interactive case studies, and virtual breakout sessions. These techniques encourage active participation and critical thinking, fostering a rich learning experience that mirrors the complexities of real-life medical scenarios.
Commitment to Continuous Education and Networking
Ongoing professional development is vital to keep educators at the forefront of educational and technological advancements. By participating in regular seminars and engaging in professional networks, educators can exchange insights and stay informed about emerging trends in telemedicine and medical education. This commitment to lifelong learning ensures that educators remain adept at delivering high-quality, impactful ACLS training in an ever-evolving digital landscape.
Step 4: Implement Pilot Programs
Pilot programs are essential for exploring the practical application of telemedicine in ACLS training. These initiatives allow for a focused examination of how telemedicine tools function within a controlled setting, providing a platform to assess their impact on training quality and delivery. Through careful planning, pilot programs can uncover potential obstacles and highlight opportunities for enhancement.
Structuring Innovative Pilot Programs
To create effective pilot programs, it’s crucial to establish specific goals and success metrics. Selecting a varied participant group, including both experienced healthcare professionals and those new to ACLS, can offer diverse perspectives on the program’s adaptability. Implementing a phased rollout, beginning with basic modules and gradually introducing more complex scenarios, allows for incremental learning and adaptation.
Leveraging Insights for Improvement
Gathering data from pilot participants is vital for refining telemedicine applications. Utilizing interviews, surveys, and observation, participants can provide detailed feedback on their experiences, shedding light on the strengths and limitations of the telemedicine approach. Comprehensive data analysis is key to understanding this feedback, focusing on the effectiveness of the telemedicine platform, user engagement, and the educational impact.
By converting insights into strategic improvements, adjustments can be made to address technical and educational challenges. This process ensures that telemedicine integration not only meets current needs but also anticipates future demands, facilitating a seamless transition to comprehensive, system-wide implementation.
Step 5: Address Challenges and Ensure Compliance
Approaching the integration of telemedicine into ACLS training involves a strategic focus on overcoming technical barriers and ensuring regulatory compliance. Identifying issues such as connectivity challenges and safeguarding privacy is crucial for maintaining the integrity of remote training. A robust framework emphasizing both technological resilience and adherence to legal standards is essential.
Tackling Technical Barriers
Reliable connectivity and technological infrastructure are pivotal for the success of telemedicine-based training programs. Ensuring robust internet connections and high-quality audiovisual capabilities supports effective communication and interaction. Implementing solutions like alternative connectivity options and offline resources can reduce potential disruptions during critical training activities.
- Network Optimization: Assess and enhance current network infrastructure to support the demands of telemedicine applications.
- Dedicated Technical Support: Establish a specialized team to provide immediate assistance and troubleshoot issues during training sessions.
Meeting Regulatory Standards
Staying compliant with evolving telehealth regulations is critical for integrating telemedicine into ACLS training. Understanding the legal requirements related to data privacy and patient confidentiality is necessary. Organizations must ensure that their telemedicine platforms implement secure data transmission protocols and maintain rigorous data protection measures.
- Regulatory Updates: Keep abreast of changes in telehealth laws to ensure continuous compliance.
- Robust Data Security: Employ comprehensive cybersecurity strategies, including encryption and access controls, to protect sensitive information effectively.
Cultivating a Security-Conscious Culture
Promoting a culture that emphasizes security and compliance involves educating all stakeholders involved in ACLS training. Regular workshops on data security best practices can empower instructors and participants to maintain these standards consistently. By fostering a culture of vigilance and responsibility, healthcare organizations ensure their telemedicine training programs meet and exceed regulatory requirements.As we navigate the ever-evolving landscape of healthcare education, the integration of telemedicine into ACLS training presents a wealth of opportunities for enhancing the skills and knowledge of healthcare professionals. By embracing innovative technologies and adaptive educational strategies, we can ensure that ACLS training remains at the forefront of medical education, equipping healthcare providers with the expertise needed to save lives in critical situations. If you’re ready to embark on this transformative journey, purchase your certification or recertification course today and join us in shaping the future of ACLS training.