Enhancing Patient Outcomes: The Role of Debriefing After ACLS Events
- Richard Barnes MD
- March 25, 2025
Post-resuscitation debriefing is a crucial practice that enables healthcare teams to reflect on their performance, identify areas for improvement, and provide emotional support to one another. By facilitating open and honest discussions immediately after a critical event, debriefings can enhance patient outcomes, promote best practices, and foster a culture of continuous learning in the medical setting.
The importance of post-resuscitation debriefing has gained increasing recognition in recent years, with organizations like the American Heart Association recommending its implementation as part of their resuscitation guidelines. However, despite the growing evidence supporting the benefits of debriefing, many healthcare institutions still struggle to make it a consistent part of their practice.
In this article, we will explore the key components of effective post-resuscitation debriefing, its impact on patient outcomes and healthcare provider well-being, and strategies for overcoming common barriers to implementation. By understanding the value of this critical process, healthcare professionals can work towards integrating debriefing as a standard of care in their organizations.
What is Post-Resuscitation Debriefing?
Post-resuscitation debriefing is a structured, facilitated discussion that takes place after a resuscitation event, such as a cardiac arrest or other critical incident. The primary purpose of debriefing is to provide a forum for the healthcare team to reflect on their performance, share perspectives, and identify opportunities for improvement in a psychologically safe environment.
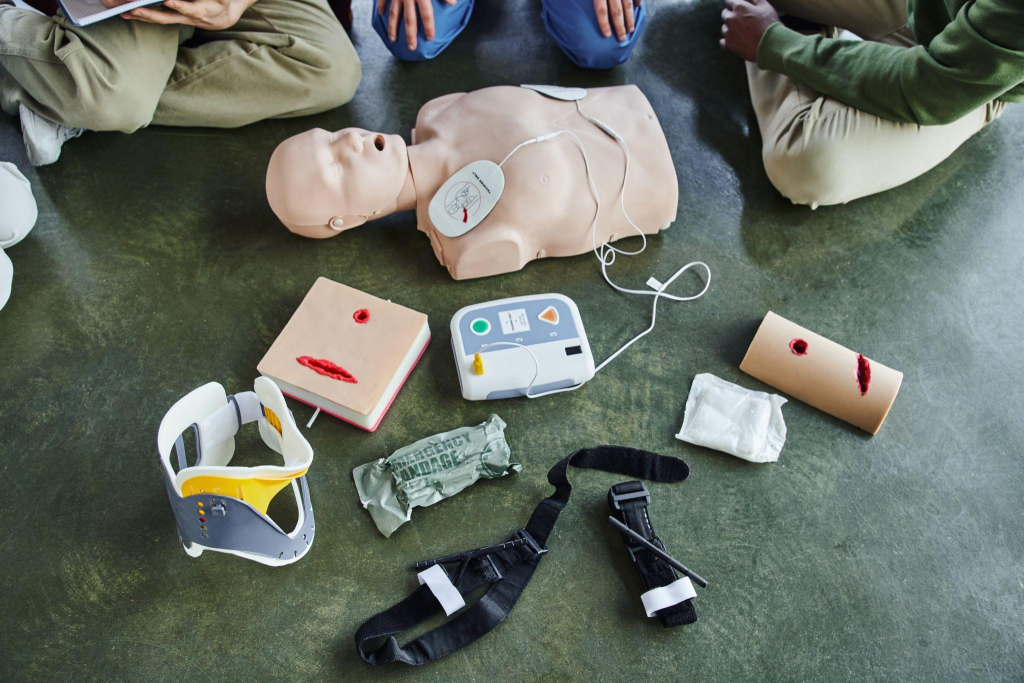
Effective debriefings typically involve all team members who participated in the resuscitation, including physicians, nurses, respiratory therapists, and other support staff. The discussion is led by a trained facilitator who guides the team through a systematic review of the event, focusing on key aspects such as communication, teamwork, clinical decision-making, and adherence to protocols, utilizing debriefing techniques in medical simulation.
One of the most important elements of successful debriefing is timing. Ideally, the discussion should take place immediately after the event, while the details are still fresh in everyone’s minds. This “hot debriefing” approach allows for a more accurate and comprehensive analysis of the situation, as well as the opportunity to address any urgent concerns or emotional needs of the team members.
By creating a dedicated space for open and honest dialogue, post-resuscitation debriefing helps to break down hierarchical barriers and promote a culture of transparency and accountability. Team members are encouraged to share their perspectives, ask questions, and provide constructive feedback to one another, with the ultimate goal of enhancing patient care and outcomes.
The Impact of Debriefing on Patient Outcomes
Debriefing after ACLS events is instrumental in uncovering system-level and process issues that can be refined to enhance future resuscitations. By engaging in a detailed examination of each event, healthcare teams can detect underlying safety threats and procedural inefficiencies, highlighting the importance of debriefing techniques for team communication. This introspective approach allows teams to implement precise modifications that streamline processes, ensuring that future resuscitation efforts are conducted with optimal efficiency and effectiveness.
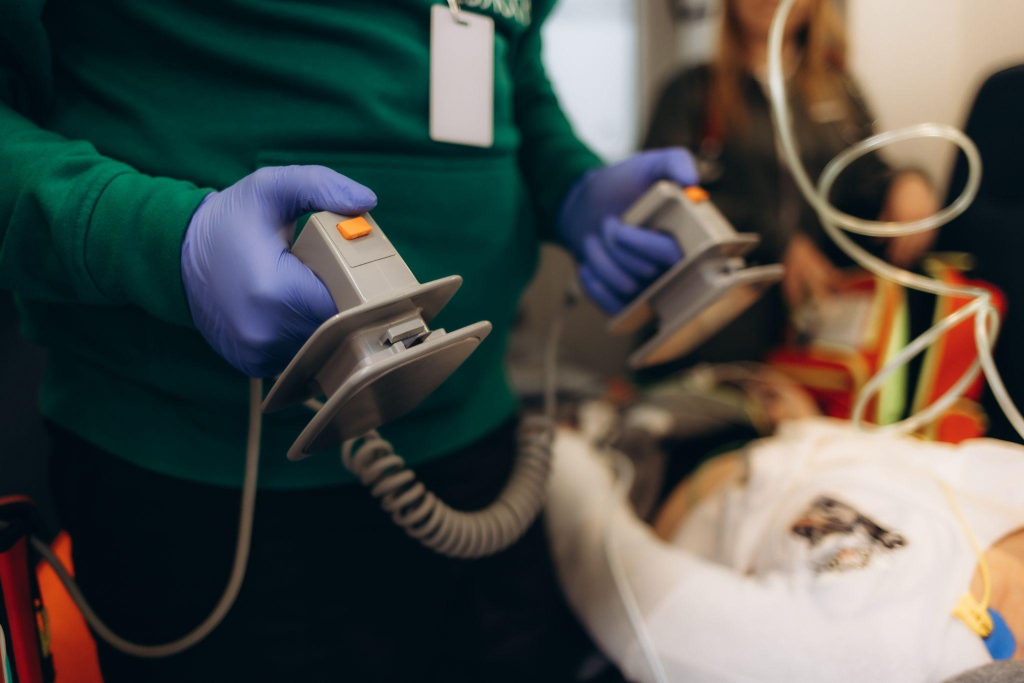
A significant advantage of debriefing is the continuous reinforcement of critical interventions, such as prompt defibrillation and timely epinephrine administration. These sessions provide the opportunity for healthcare providers to reinforce these interventions, keeping them central to their clinical practice. This focus not only strengthens clinical proficiency but also contributes to higher patient survival rates by emphasizing the execution of proven interventions during high-pressure situations.
Potential to Improve Resuscitation Quality Metrics
Debriefing plays a pivotal role in boosting adherence to ACLS protocols and guidelines. Through a comprehensive review and discussion, teams can pinpoint instances of protocol deviation and explore the underlying causes. This understanding fosters a disciplined approach to maintaining protocol fidelity, thus elevating the chances of successful patient outcomes.
Furthermore, debriefing improves team dynamics and communication during critical situations. By evaluating the interaction and coordination during resuscitation, teams can identify communication gaps or role uncertainties that may have impeded performance. Addressing these challenges in a constructive setting enables the development of strategies that enhance team integration and clarify roles and responsibilities, ensuring readiness when critical moments arise. This elevated level of preparedness and team synergy directly influences the success of resuscitation efforts, leading to superior patient care.
Debriefing and Healthcare Provider Well-being

Debriefing sessions offer a structured setting where healthcare teams can collectively address the emotional turmoil inherent in high-stakes resuscitation events. These gatherings promote a supportive network, allowing team members to share experiences and insights, which contributes to their psychological resilience. By fostering a culture of mutual support and reflection, debriefing helps healthcare professionals navigate the emotional challenges of their roles.
The aftermath of resuscitation efforts can leave healthcare providers grappling with emotional distress, often described as the “second victim” phenomenon, which can be addressed through psychological debriefing for post-traumatic stress disorder. This emotional strain, if unaddressed, may lead to burnout, a common issue in the medical field. Incorporating debriefing into routine practice allows teams to openly discuss these challenges and seek collective solutions. This proactive engagement supports mental well-being and enhances the ability of providers to deliver empathetic, effective care.
Strategies to Provide Psychological Safety During Debriefing
Ensuring psychological safety during debriefing is crucial for encouraging honest dialogue among team members, as outlined in the standards for the debriefing process in healthcare. Focusing on systemic challenges rather than individual shortcomings helps maintain a non-judgmental environment, enabling participants to concentrate on procedural enhancements. This approach cultivates a learning-oriented atmosphere, where team members feel comfortable contributing to the discussion.
Recognizing the intense pressure and complexity of resuscitation events is vital in promoting psychological safety. Acknowledging these realities reassures healthcare providers that their emotional responses are valid and understood. This recognition encourages full engagement in debriefing, as individuals feel their perspectives are valued and respected.
Enhancing psychological safety can also be achieved by offering access to supportive resources. Institutions can provide counseling services or implement peer support programs to extend emotional support beyond debriefing sessions. Such comprehensive support systems empower healthcare providers to manage the emotional demands of their work, contributing to their overall job satisfaction and well-being.
Overcoming Barriers to Implementing Debriefing

In healthcare environments where rapid transitions are the norm, integrating debriefing into routine practice faces obstacles such as limited time and competing demands. The urgency to attend to successive patients or tasks often overshadows the need for reflective practices, leading to the neglect of debriefing opportunities that could significantly improve performance. Moreover, the absence of standardized procedures and facilitators skilled in guiding debriefings can hinder the effectiveness of these crucial sessions. Without a consistent framework and expert guidance, debriefing discussions may lack focus and fail to yield actionable insights, diminishing their potential benefits.
Discrepancies in how debriefings are conducted across different units or institutions further complicate implementation, resulting in a fragmented understanding of effective debriefing. Establishing comprehensive guidelines and developing facilitator training programs are essential steps in overcoming these challenges. This approach ensures that all team members can participate in meaningful and productive debriefings, fostering a culture of continuous improvement and excellence in patient care.
Practical Solutions for Conducting Efficient Debriefings
To address these challenges, healthcare organizations can adopt practical strategies that streamline the debriefing process. Implementing structured tools such as the DISCERN framework provides a clear pathway for discussion, aiding facilitators and participants in systematically exploring key aspects of resuscitation events, following steps to evaluate training sessions through debriefing. This structured approach ensures that critical points are addressed, enhancing the overall effectiveness of debriefings.
Appointing debriefing champions within each unit can also promote the practice by acting as advocates for reflection and improvement. These champions play a pivotal role in encouraging participation and maintaining focus on the value of debriefing. By embedding this culture into daily operations, champions help integrate debriefing as a natural part of the resuscitation process.
Incorporating efficient strategies like “hot debriefs” allows teams to capture insights immediately following an event, minimizing recall bias and reinforcing important lessons. This immediacy leverages fresh perspectives, enabling teams to identify improvement areas promptly. By adopting these strategies, healthcare teams can maximize the impact of debriefing, ultimately enhancing both team dynamics and patient outcomes.
Debriefing as a Quality Improvement Initiative

Debriefing provides a unique opportunity to drive quality advancement in healthcare settings. Through comprehensive evaluations of resuscitation events, debriefings allow teams to uncover overlooked risks that may jeopardize patient safety. By addressing these potential issues early, healthcare providers can implement preventive measures that enhance overall safety protocols. Additionally, debriefings often highlight the need for more resources or specialized training, offering a clear direction for strategic development and capability building.
The integration of insights from debriefings into broader quality enhancement initiatives is critical for sustained improvement in patient care. Utilizing a systematic approach to collect and analyze debriefing data enables healthcare organizations to translate these insights into practical strategies. This evidence-based approach not only identifies recurring challenges but also helps in prioritizing interventions that deliver significant improvements in care delivery. Aligning debriefing outcomes with strategic objectives ensures that efforts are both effective and aligned with the organization’s mission.
Integrating Debriefing Data into Resuscitation Quality Reviews
Incorporating debriefing data into resuscitation quality reviews provides a comprehensive understanding of clinical effectiveness. By including these insights in morbidity and mortality evaluations, healthcare teams can engage in detailed discussions that assess both clinical outcomes and operational efficiencies. This integration promotes a collective learning environment where the focus is on continuous improvement rather than individual performance, fostering a culture of collaborative growth and accountability.
Regular analysis of debriefing data can reveal underlying trends and patterns that may not be evident in isolated assessments. By consistently evaluating these trends, healthcare organizations can identify ongoing issues and address them through targeted strategies. This proactive approach ensures that quality improvement initiatives remain adaptable and responsive to the changing needs of both patients and healthcare providers, fostering an enduring commitment to excellence in patient care.
Best Practices for Maximizing the Value of Resuscitation Debriefing
Embedding debriefing into the fabric of clinical practice involves more than mere routine—it requires strategic integration that aligns with institutional goals. This integration means crafting a debriefing protocol that is adaptable yet consistent, ensuring it becomes an expected and valuable part of the resuscitation process. By doing so, healthcare teams can cultivate a culture of reflection that naturally leads to improved patient care and team performance.
Incorporating a wide array of professional insights during debriefings is essential for capturing the full spectrum of experiences and challenges encountered during resuscitation. This approach involves actively seeking contributions from various disciplines to construct a holistic view of the event. Such diversity in perspectives not only uncovers unique insights but also strengthens interprofessional collaboration, fostering an environment where diverse ideas are valued and leveraged for better outcomes.
Accountability and Implementation
A crucial aspect of maximizing debriefing effectiveness is the transition from discussion to action. Establishing clear pathways for implementing changes based on debriefing discussions ensures that insights translate into practice improvements. Assigning specific roles and responsibilities for action items helps maintain accountability and drives the momentum needed for sustained change.
To support this, maintaining a comprehensive record of debriefing discussions and the resulting action steps is vital. This documentation acts as a benchmark for evaluating progress and success, providing a feedback loop that informs ongoing quality improvement efforts. By committing to these practices, healthcare teams can leverage debriefing not just as a tool for reflection, but as a catalyst for enduring enhancements in patient care delivery.
In conclusion, debriefing after ACLS events is a critical practice that enhances patient outcomes, supports healthcare provider well-being, and drives continuous quality improvement. By embracing the power of reflection and implementing best practices, healthcare teams can unlock the full potential of debriefing as a catalyst for positive change. If you’re ready to elevate your skills and contribute to a culture of excellence in patient care, we invite you to explore our online certification and recertification courses at Affordable ACLS and take the first step towards making a lasting impact in the lives of your patients.