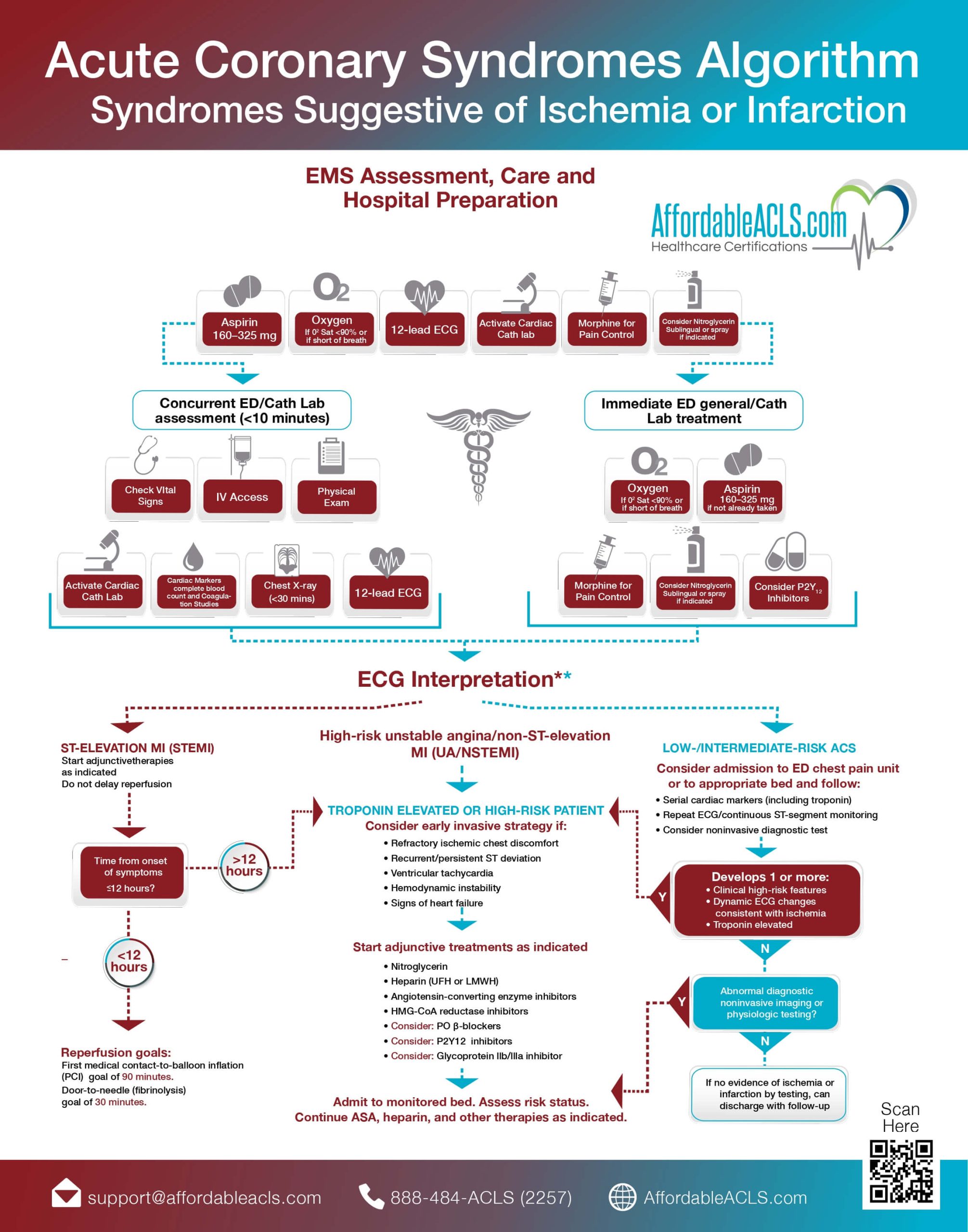
In the presence of ACS, EMS or the Emergency Department will start with care and prioritize getting a 12-lead ECG, giving aspirin, and oxygen therapy if oxygen saturation is <90% (or if the patient is short of breath) administering nitroglycerin, if not hypotensive and/or morphine for discomfort, , and most importantly, activating the cardiac cath lab. In the initial minutes of care, the patient will have vital signs taken, get IV access, and have a physical exam. The ED will obtain labs, including high sensitivity troponins (hs-Trop). A chest x-ray should also be completed.
If the patient is having an ST-elevation MI (STEMI), adjunctive therapies must be started immediately with the goal of reperfusion as soon as possible. If the STEMI has evolved in less than 12 hours, the goal from first medical contact to the balloon inflation (FMC-to-balloon) is 90 minutes. The goal of door-to-fibrinolysis is 30 minutes.
An NSTEMI indicates there is no ST segment elevation, however, ischemia is still likely, and cardiac markers such as high sensitivity troponin are usually elevated. Serial troponins are normally obtained.
The algorithm above outlines this workflow, and gives medical personnel steps to take in the event of ACS (Acute Coronary Syndrome).
- Pre-Hospital
Perform an assessment of chest discomfort suggestive of ischemia or infarction while transporting the patient to an appropriate facility, monitor and support airway, breathing, and circulation, providing CPR and defibrillation if needed. Administer aspirin, and provide oxygen if saturation levels are below 90%. Consider the use of nitrates.Obtain a 12-lead ECG. EMS will call the hospital if ST elevation is identified. Notified hospital should mobilize hospital resources to respond to STEMI. Complete a fibrinolytic checklist if it’s indicated.
- Hospital (Emergency Department)
Assessment and stabilization of the patient should occur within the first 10 minutes of arrival at the emergency department. 12 lead EKG immediately. Assess the patient’s vitals and oxygen needs and establish an IV. Obtain history and physical exam. Check for contraindications for fibrinolytic therapy if indicated, and obtain initial troponin. If oxygen saturation is below 90%, start oxygen at 4 liters per minute. Administer 325 milligrams of aspirin. Administer nitrates for chest pain if indicated. Consider morphine. Order chest x-ray.
EKG will be either: ST-elevation myocardial infarction, or STEMI; non-ST-elevation acute coronary syndrome (NSTEMI); low to intermediate risk acute coronary syndrome, or normal.
A. ST-elevation MI (STEMI). If ST elevation or new or presumably new lower bundle branch block is detected, begin treatment for STEMI. For EMS providers, activate a STEMI alert with the receiving hospital as soon as possible.
Time from onset of symptoms < 12 hours. If the time from onset of symptoms is 12 hours or less, proceed with reperfusion therapy. If the time from onset is greater than 12 hours, treat as a troponin elevated or high-risk patient.
Reperfusion. Door to balloon time is 90 minutes. The door to needle goal for fibrinolysis is 30 minutes.
B. Non ST elevation MI (NSTEMI-ACS). Usually characterized by refractory chest pain, elevated troponin, and non-specific ekg changes such as t wave inversion.
Cardiac catheterization should be considered if they are experiencing refractory chest pain, recurrent ST depression or change, low blood pressure, ventricular tachycardia, pulmonary edema. Administer nitroglycerin / heparin.
C. Low- or intermediate-risk ACS. If changes in the ST segment or T-wave are normal or nondiagnostic, begin treatment for low- or intermediate-risk patient. Consider admission to the ED chest pain unit. Monitor, cardiology consultation, serial troponins, serial ekgs, aspirin.